October 10, 2025
As the US government is in its second week of being shut down, the ripple effects across global health shows the interconnectedness of the public health infrastructure in the US and globally and uncertainty about the future of foreign aid. Amid this turmoil, the World Health Organization has prequalified injectable lenacapavir for PrEP in record time, using a new, expedited process. This development marks an important bright spot, signaling momentum toward broader HIV prevention access.
WHO Prequalifies Oral and Injectable Lenacapavir
The World Health Organization (WHO) prequalified both the oral tablet and injectable forms of lenacapavir (LEN) for PrEP. The prequalification was done through a new, expedited prequalification pathway that can facilitate national registration through the Collaborative Registration Procedure for Prequalified Products (CRP-PQ), which may streamline access to these products beyond the traditional approval routes. WHO prequalification followed the European Medicines Agency’s (EMA) positive scientific opinion and happened 36 days after filing. As Meg Doherty, WHO’s Director of Science for Health and former visionary director of WHO’s Global HIV, Hepatitis and STI Programmes, pointed out, this is the first example of 12-month alignment of WHO guidelines and prequalification of a product within 12 months of the clinical trial evidence.
IMPLICATIONS: This milestone represents major advances in speeding access for global HIV prevention. The speed and flexibility of WHO’s accelerated process represents regulatory innovation that can accelerate access to essential health products. For lenacapavir, prequalification means that countries may be able to move more quickly through the process of licensing and delivering the product with fewer regulatory barriers and faster timelines. Now, other aspects of the delivery chain – procurement, supply chains, equitable distribution mechanisms, demand creation, monitoring and evaluation and implementation science – need to adapt this commitment to speed in reaching large-scale impact.
READ:
- First lenacapavirs prequalified—WHO
- The six-monthly anti-HIV jab is coming. But can SA keep track of millions of users?—Bhekisisa
- Panel Discussion: The Role of Basic Science, Global Clinical Trials and Community Engagement in the Development of Lenacapavir—24 Hours to Save AIDS Research marathon
US CDC Deleted Critical Health Information from Websites Silently
The decisions and actions at the US Centers for Disease Control and Prevention (CDC) continue to spiral downward. Earlier this week, key public health content was removed from its websites, including guidance on HIV and STI prevention, testing, and treatment. These deletions occurred without notice or explanation, which prompted public health leaders and organizations, including AVAC, to condemn the actions: “Removing these resources undermines transparency, public trust, and efforts to eliminate health disparities, especially for communities most affected by these epidemics.”
IMPLICATIONS: The CDC’s quiet removal of crucial HIV and STI content has not been done in isolation. We’ve witnessed a quick erosion of scientific leadership and transparency and an uptick in mis-information. Together, these actions continue a troubling shift, where political agendas override scientific transparency.
READ:
- HIV, STI Leaders Condemn the Recent Deletion of Critical Public Health Information From CDC Websites—POZ
NIAID Initiates Network Renewal Process
The US National Institute of Allergy and Infectious Diseases (NIAID) initiated a public consultation to gather feedback on the future of its four Division of AIDS (DAIDS)-sponsored HIV clinical research networks: the AIDS Clinical Trials Group (ACTG), International Maternal Pediatric Adolescent AIDS Clinical Trials Network (IMPAACT), HIV Prevention Trials Network (HPTN), and HIV Vaccine Trials Network (HVTN). The goal of this process is to incorporate external perspectives from researchers, advocates, and others into the planning and renewal of network cooperative agreements and the priorities they reflect. These agreements are set to be recompeted in 2026 and awarded for the 2027–2034 cycle.
IMPLICATIONS: The NIH has a longstanding mandate to advance fundamental scientific knowledge. Many of the most transformative innovations in HIV prevention and treatment are the direct result of decades of NIH investments in the clinical trial networks. This mandate must be protected and strategically resourced, even amid broader funding pressures. An evidence-based, balance research portfolio, including robust clinical trial infrastructure globally, is essential to ending the HIV/AIDS epidemic in the US and around the world.
READ:
- AVAC Input for Recompetition of the NIAID HIV/AIDS Clinical Trials Networks—AVAC
- TAG’s Recommendations to NIAID on the Future of the HIV Clinical Trials Networks—TAG
- Panel Discussion: HIV Clinical Trials and Research Networks—24 Hours to Save AIDS Research marathon
Inclusion Made Simple, In Difficult Times
“Not even a week after the American Journal of Public Health published our paper, Addressing Transgender Erasure in HIV Clinical Trials, the US NIH moved to prohibit scientists from collecting data about gender,” write HANC’s Brian Minalga and AVAC’s Cindra Fuerer in a new blog post.
What We’re Reading
- The Global Fund works—these stories remind us why it’s essential—Gates Foundation
- The global health landscape will never be the same — and it shouldn’t be—Devex
- Inside the EU’s private assessment on Trump’s massive aid cuts—Euractiv
- US ‘undermining global health’ by threatening to strip funding from aid projects that do not fit its political agenda—The Guardian
- How the Trump administration learned to love foreign aid—The Economist
- The Fallout From the Dismantling of USAID Continues—Newsweek
- ‘Trump plans to block funding to groups who promote diversity policies abroad—Politico
- The impact of cuts in the US President’s Emergency Plan for AIDS Relief funding for HIV pre-exposure prophylaxis in sub-Saharan Africa: a modelling study—Lancet HIV
- Supporting RECs/IRBs to Review the Enrolment of Pregnant/Lactating Individuals in HIV Prevention Trials using International Ethical Guidance—Research Ethics
- WHO launches the Global Clinical Trials Forum—WHO
- Broader access urged for affordable HIV drug—SciDevNet
- CDC, its advisers quietly expand access to Covid-19 shot for pregnant women—Politico
- US aid cuts are being felt across Africa. Here’s where.—Washington Post
- New study shows all-in-one coronavirus vaccines could save millions of lives in future pandemics—CEPI
- ‘Bluetoothing’: Blood-Sharing Drug Trend Fuels Alarming Global HIV Surge—New York Times
AVAC Resources
- Lenacapavir Regulatory Approval
- Potential Demand for LEN for PrEP
- HIV Prevention Product Overview
- Where We Are Now With LEN
- PrEP Price Comparison
Upcoming Webinar
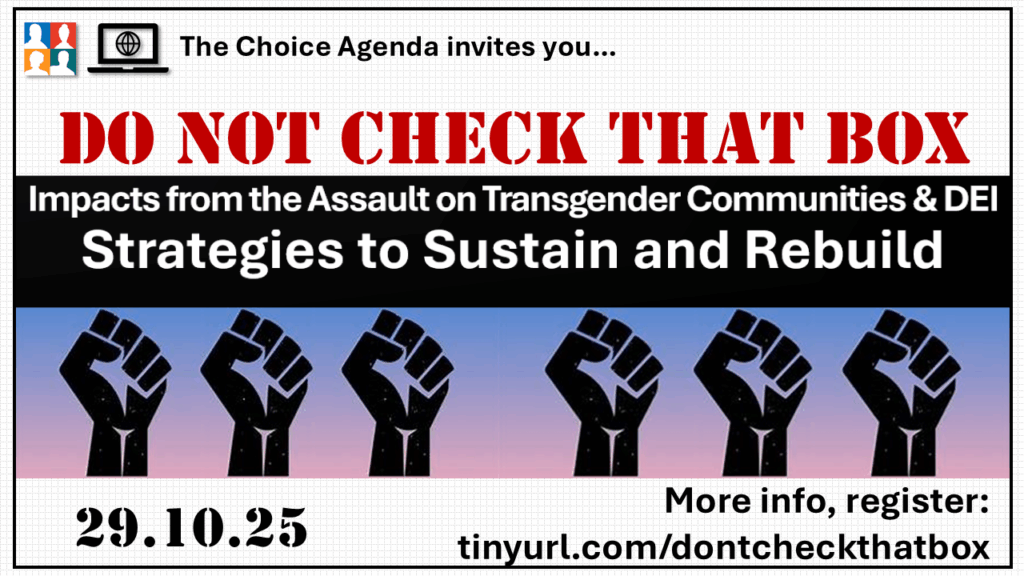
Presented by The Choice Agenda: join our panelists for an unflinchingly honest—and interactive—conversation as we assess the impacts of the ongoing assault on transgender communities, gender affirming health care, data collection, and Diversity, Equity and Inclusion writ large. Strategies to restore trust, sustain programming, and rebuild from the ashes will be explored.