The United States Agency for International Development (USAID) is seeking applications from qualified U.S. and Non-U.S. organizations to fund a project entitled “Advancing the development and licensure of vaginal rings and innovative systemic methods for prevention of HIV infection in women”. For more information click here.
Advancing the development and licensure of vaginal rings and innovative systemic methods for prevention of HIV infection in women
Dapivirine Ring—Past, Present and Future
AVAC’s new issue of Px Wire is an advocate’s guide to the past, present and future of the dapivirine ring for HIV prevention. It features a timeline of key milestones that could lead to licensure, a simple comprehensive Q & A, and a closer look at where sub-Saharan African women will have access to daily oral PrEP and/or the Ring via open-label extension studies. We hope this resource will be used to spark discussion and guide plans for further engagement.
Click to download the new issue of Px Wire.
The full issue of Px Wire, as well as our archive of old issues and information on ordering print copies, can be found at www.avac.org/pxwire.
Introducing Implementation and Access Resources on PrEP Watch
Daily oral PrEP is moving from an idea to an offering in more countries and communities every day. And in the places where it isn’t being offered, demand is growing!
To help advocates track implementation on the ground in detail, AVAC has developed a new section of PrEP Watch (a clearinghouse of information on PrEP science, research, cost, access and advocacy) focused specifically on implementation efforts underway.
On the Implementation Initiatives page, you can find information about some of the different initiatives funding PrEP implementation in sub-Saharan Africa, including the USAID-supported OPTIONS Consortium and the PEPFAR DREAMS Initiative. Information about funder-defined initiatives can help advocates understand who’s who and what’s planned—and to follow the money!
You can also learn about the full spectrum of work happening at country level in Kenya, South Africa and Zimbabwe. As PrEP is rolled out in additional countries, more case studies will be added.
PrEP Watch will continue to grow as PrEP introduction and rollout moves forward and as new efforts and initiatives are started.
Reach us at [email protected] if you have comments or questions.
Antibody Research Advances to Prevention Efficacy Trial(s): An Advocates’ Perspective
This week the NIH-funded HIV Vaccine Trials Network (HVTN) and HIV Prevention Trials Network (HPTN) announced the launch of the HVTN 704/HPTN 085 trial, also known as “AMP” (Antibody-Mediated Prevention). The Phase IIb trial is designed to measure the safety and effectiveness of an intravenous infusion of the broadly neutralizing antibody VRC01 for HIV prevention. The infusion will be delivered to participants every eight weeks over the course of a year and a half (participants are also followed for 20 weeks after their last infusion).
AMP consists of two parallel trials conducted collaboratively by the the HVTN and HPTN. The trial that just initiated (HVTN 704/HPTN 085) has 24 sites across Brazil, Peru and the US and plans to recruit 2,700 men and transgender people who have sex with men. The other study, HVTN 703/HPTN 081, will be initiated later this year and will enroll 1,500 women at 15 sites across Botswana, Kenya, Malawi, Mozambique, South Africa, Tanzania and Zimbabwe.
For the past several years, scientists have been working with potent antibodies that neutralize many different strains of HIV. These broadly neutralizing antibodies, or bNAbs, include VRC01. Antibodies are substances made by the immune system; these bNAbs have been isolated from people living with HIV. Researchers have purified the bNAbs and modified them to make them even more effective against HIV. The antibodies in trials like AMP are delivered via infusion—meaning intravenous administration. The approach of delivering an immune defense directly is called passive immunization, and it stands in contrast to vaccination or immunizations that teach the body how to mount an immune defense itself, via a vaccine. In the AMP trial study visits are expected to take approximately 90 minutes and participants are scheduled to come to the clinic every eight weeks.
Many scientists in the field say that the point of bNAb trials isn’t to identify a new strategy for widespread use. Instead, a positive result could lead to more focused vaccine development efforts. Other researchers say that more potent antibodies that could protect in smaller, more easily-administered doses, could perhaps make it to market one day. For this to happen, all agree that the dosage (the amount delivered to a person) would need to come down from where it is in the AMP trial, and the half-life (a measure of the time that protective levels of antibody stay in the blood) would need to go up.
The AMP trials will contribute significantly to the field’s understanding of how to fight HIV. AVAC and other advocates have urged that the trial sponsors and implementers ensure consistency in the messaging about and expectations for VRC01—especially given that other, more potent antibodies may be ready for additional testing by the time the AMP trials are over, alone or in combination. (This is a common conundrum in research: first-in-class products break new ground but may not be the optimal choices for introduction.)
Extensive and continuous stakeholder engagement is essential to ensure that passive immunization trials and product development plans are clearly articulated.
The AMP trials are among the first prevention efficacy trials to start in the “post-PrEP-approval” era, raising an issue that’s challenging prevention stakeholders everywhere: the need to define the standard of prevention in trials to include daily oral PrEP, which is now recommended by the WHO for all people at substantial risk of HIV. People who participate in efficacy trials are, by definition, at substantial risk of acquiring HIV and therefore there is an ethical imperative to include PrEP. The question is how—and how to design trials that can answer questions about new products, even as incidence may go down due to PrEP use.
The AMP trial that launched this week has this to say about its approach to PrEP:
“Volunteers in the AMP Studies will be referred to available local programs where they may obtain the oral medication Truvada [TDF/FTC] to take daily for HIV prevention, a highly effective practice called pre-exposure prophylaxis (PrEP). Volunteers’ access to PrEP will expand as more host countries approve Truvada for PrEP and develop the infrastructure to support its use.”
The prevention standard of care is defined as, “condoms and lubricant, counseling on how to reduce behaviors that increase risk for infection, and counseling and referral for antiretrovirals to take immediately following suspected exposure to HIV (post-exposure prophylaxis).”
ACT UP New York member and long-time activist Luis Santiago responded, “Should Truvada/PrEP be more than just an ‘option’? Should it be actually provided in the studies in the control arm? Are we back to the ethical discussion of the 1990s?”
These questions, which were a key part of the prevention advocacy agenda years ago, still apply today—how does the field ensure that trials are not responsive to context but help to shape it? There is precedent for this, as the HVTN ensured access to antiretroviral therapy for individuals who seroconverted in vaccine trials before ART was widely available in Africa, and subsequently ensured access to voluntary medical male circumcision (VMMC) in its vaccine trial in South Africa before there was national policy on that strategy.
The reality of HIV prevention programming is rapidly evolving. In just the past four months, three of the AMP trial host countries (Kenya, Peru, South Africa) joined the US in approved TDF/FTC for daily oral PrEP, joining the USA in this decision. This leaves six AMP countries that have not: Botswana, Brazil, Malawi, Mozambique, Tanzania and Zimbabwe. But approval doesn’t mean access, and these countries may or may not have programs set up to which AMP participants can be easily and effectively referred. In that case, it’s up to the trial site to sort out provision of this key service.
At the end of the day, everyone is after the same thing—access to new options that can prevent HIV today and in the future, whether that’s a pill in hand for a young woman at risk today or a vaccine or antibody for the generations to come.
Additional Information
John Mascola of the Vaccine Research Center (VRC) that isolated the VRC01 antibody recently presented on the use of antibodies for both prevention and treatment, which provides helpful background and context for these recent developments, Harnessing Antibodies for HIV Prevention and Treatment.
Additional study info can be found in AVAC’s prevention research and development database (PxRD) and at ampstudy.org.
WHO Writes Back…Five Months Later: An update on HC-HIV advocacy
A nearly five-month long waiting game for a response from the World Health Organization (WHO) regarding advocates’ concerns about its confusing and inaccurate statement on the relationship between some forms of hormonal contraception and HIV ended on April 5. Sadly, the response starts a new waiting game, since the long-awaited letter promised action on some, though not all, of the points raised in the original letter (sent November 12, 2015), with no timeline or process described for taking that action. (Wheels may be turning, as the link to the October 2015 statement no longer goes to the full statement.)
By way of background, in October 2015, the WHO, without warning, posted a new statement on hormonal contraception and HIV on its website. The statement claimed to be a clarification of the existing, expert-reviewed guidance on the topic. However, it contained a range of inaccurate and confusing statements that contradicted or muddied the clarity of the statement it sought to simplify.
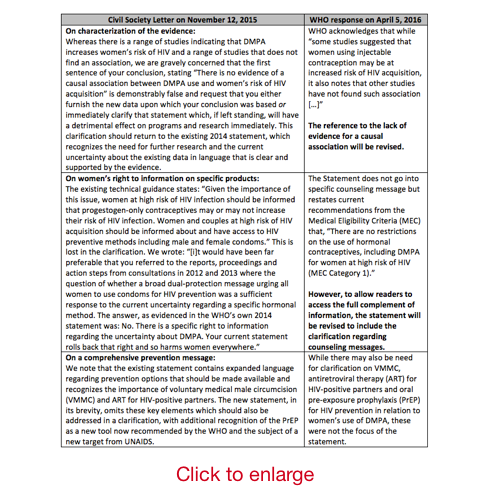
On November 12, 2015 an international coalition of organizations wrote an urgent letter to the WHO requesting immediate action on the statement. Citing the confusion that the new statement caused in terms of the mixed evidence showing that DMPA, aka Depo-Provera, impacts women’s risk of HIV, advocates asked for the statement to be taken down so that the existing note would continue to be the main point of reference for the field. The letter was sent by the International Community of Women Living with HIV Eastern Africa (ICWEA), co-convener of a civil society working group on contraception and HIV, and AVAC. (You can read the original sign-on letter here, and see a table below that outlines the requests in that letter with the WHO response).
The letter wasn’t officially acknowledged until some months later, when ICWEA wrote requesting an update. And the response did not come in until April 5. In summary, WHO agreed to:
(1) revise the statement to correctly characterize the evidence;
(2) revise the statement to specifically reference women’s right to know about the uncertainty regarding DMPA and HIV risk.
WHO stated that it will not add reference to additional prevention methods beyond male and female condoms, even though the technical guidance refers to a range of methods. This is particularly disappointing given WHO’s strong recommendation in September for the offer of oral PrEP for “all people at substantial risk of infection”.
ICWEA and AVAC will work with partners who signed on to the original response to develop a response in the coming days. Please be in touch with ideas and reactions.
Below is what we asked for and what WHO said, in detail: