This HIV Vaccine Awareness Day, AVAC has an updated toolkit of resources for translating HIV vaccine research with a renewed sense of urgency, and two dedicated hashtags to rally the call on social media: #HIVvaccineAware and #HVAD2019. We hope you’ll join the conversation — with the updated HVAD 2019 toolkit and our upcoming webinars!
Mitchell Warren is Executive Director of AVAC. This post first appeared in Science Speaks.
This year’s annual HIV Vaccine Awareness Day arrives Saturday at a promising and also perilous time for vaccines.
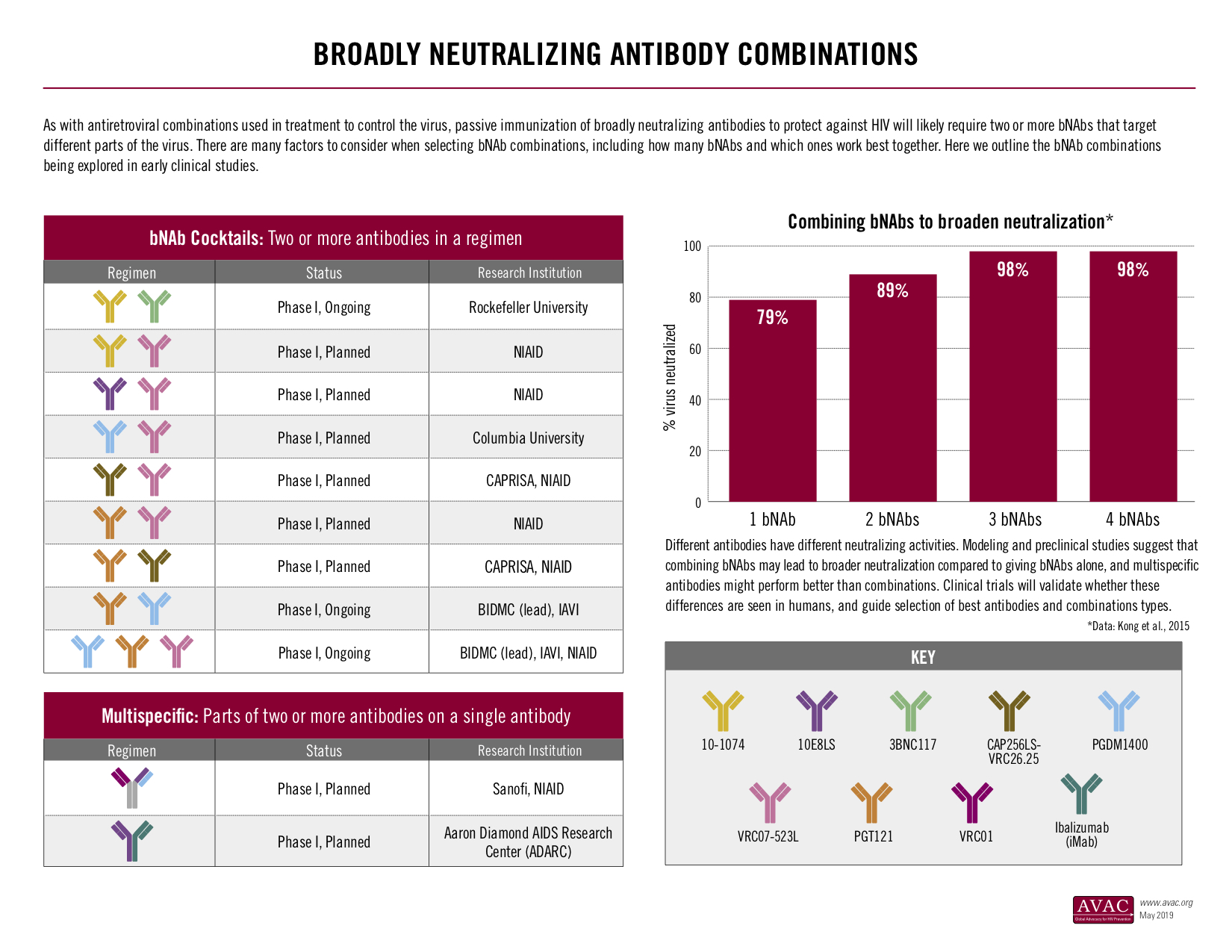
On one hand, multiple vaccine candidates that might protect against HIV are advancing in large clinical trials. Thanks to an extraordinary global commitment and US government investment, two large-scale studies testing different HIV vaccines are underway in Africa, and a third trial is slated to start soon in the Americas and Europe. Simultaneously, researchers are advancing other promising approaches in the lab, such as those that harness powerful anti-HIV antibodies to protect against the virus.
This golden age of vaccines is not limited to HIV. Infants in three African countries will soon receive a vaccine designed to reduce malaria — a disease that kills one child every 30 seconds, according to UNICEF. A vaccine to prevent pulmonary tuberculosis in adults may soon advance to a large-scale trial and could become a central component of strategies to contain this life-threatening disease that, when left untreated, kills half the patients it affects. And an experimental Ebola vaccine is being deployed with urgency to stop a growing outbreak in the Democratic Republic of the Congo.
Vaccines have changed our lives in fundamental ways. In many parts of the world, vaccine-preventable diseases that terrified our parents and grandparents are dim memories today. But vaccines are not simple products. Many have challenges. Some are hard to manufacture; some only provide temporary or partial protection. Improving vaccines, using them effectively, educating potential users and ensuring that vaccines reach those in need all require public support and engagement.
Today, however, a rising global tide of anti-vaccine misinformation and sentiment is challenging that informed engagement — with potentially deadly results. Anti-vaccine fervor, based on discredited pseudo-science and too often endorsed by religious, government or community leaders, has led to the resurgence of diseases, such as the current — and completely preventable — measles outbreak, that were once considered conquered.
The implications of the anti-vaccination movement are enormous. Just as vaccines against some of the greatest global killers finally come within reach, fear and misinformation could diminish vital commitments to continued vaccine research, and important investments in vaccine education and delivery. Effective vaccines might not get developed, manufactured, distributed or used due to misguided, anti-vaccine sentiment — potentially putting millions of people at risk for entirely preventable deaths and diseases.
In the case of HIV, a faltering commitment to a vaccine would be devastating. Even with highly effective treatment and a daily prevention pill (known as PrEP) that can reduce HIV infections by more than 95%, nearly 2 million people still become infected with HIV each year. In the United States, a government pledge to end the domestic epidemic must confront the reality of an HIV infection rate that has barely changed since 2013. And in many parts of the world, new HIV infection rates, especially among vulnerable and marginalized populations, are actually rising rather than falling. All of these statistics point to one undeniable truth: we have made important progress against HIV, but this epidemic will not end without a vaccine.
In labs around the world, vaccine researchers are doing what we’ve asked them to do…making unprecedented progress against some of the most complex pathogens ever targeted.
Now, we must all leverage that scientific progress to rebuild a vital component of public health – faith in and support for vaccines. New vaccines in development present the greatest opportunity to save lives in human history. We cannot allow that opportunity slip away due to indifference, neglect or misinformation.
This HIV Vaccine Awareness Day, it’s time for a renewed global commitment to vaccine research, development and delivery. Vaccines save lives today, and a new generation of vaccines can save even more lives tomorrow.