Last week’s 30th Conference on Retroviruses and Opportunistic Infections (CROI) showed an energized field- with scientific advances galvanizing research across a host of disease areas. The findings highlighted in this round up offer a look at standout research — and, at AVAC, we know it must be matched with informed advocacy.
Scroll down to learn about new interventions for sexually transmitted infections (STIs), expanding evidence for widespread use of long-acting products for HIV prevention, pipeline updates for user-controlled short-acting products for HIV prevention, new insights about the impact of mpox, discussion of what’s ahead for HIV vaccine science and more.
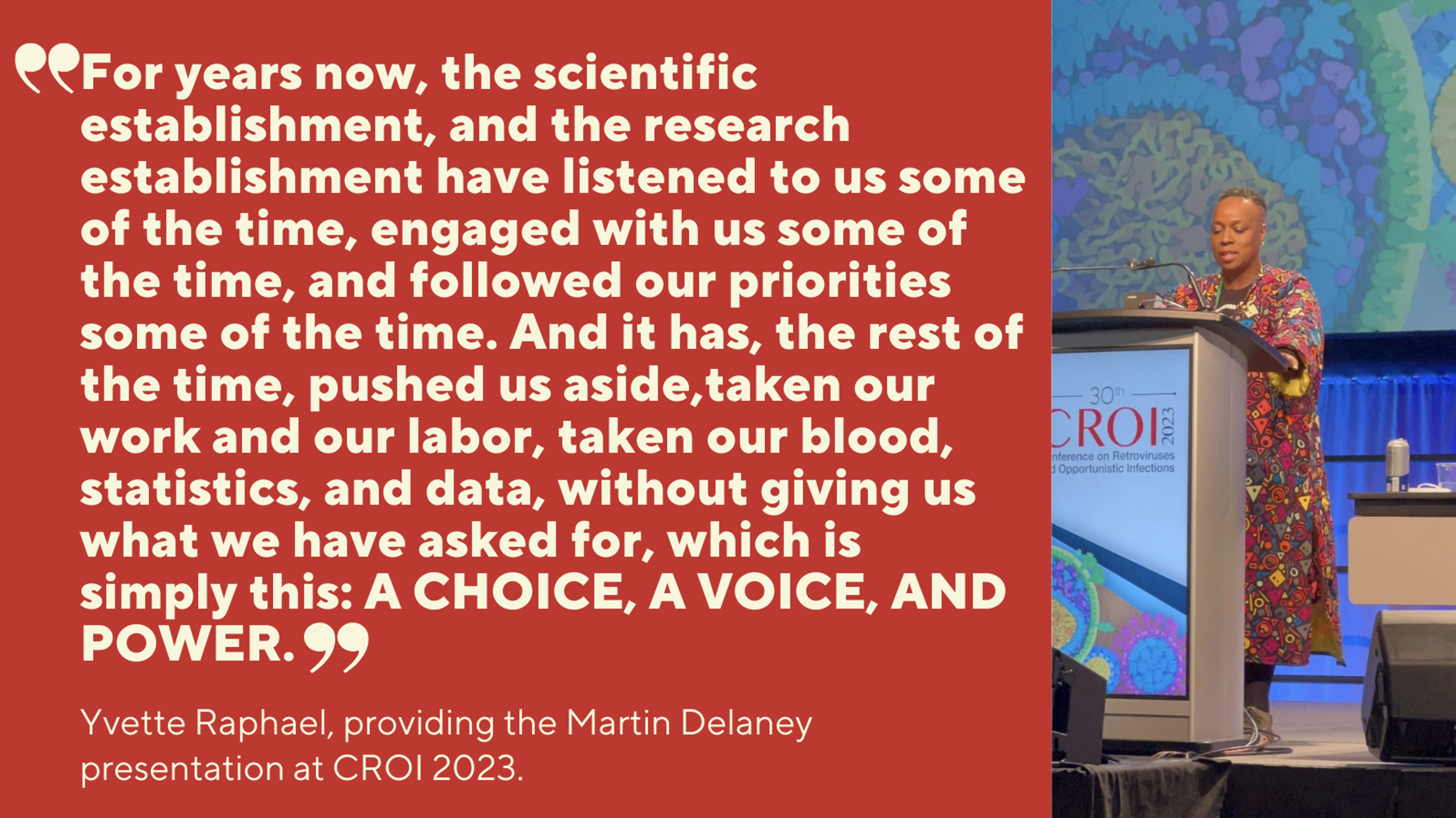
To put it all in context, CROI’s opening session included two unforgettable voices: former head of NIAID, Anthony Fauci recounted 30 years of struggle and progress toward HIV treatment, prevention and cure; and APHA’s Yvette Raphael, a passionate advocate and long-time AVAC partner, connected the science to the advocacy — particularly the relentless efforts of African women — to fight for justice, equity, access and inclusion in research, planning and programs (check out our Advocate’s Network from last week for more on this incredible opening session and watch it here). Yvette’s message was ringing through every CROI session. It informed the ever-popular Margarita Breakfast Club sessions over Zoom (find the recordings and other resource materials here), where connecting the science and the advocacy happened early every morning before CROI’s opening plenary, because pioneering science is only half the effort. It’s fierce advocates and tireless advocacy that brings the fruits of science to those who need them most.
So, read on and get ready.
Table of Contents
- DoxyPEP for STIs, and a Vaccine for Gonorrhea: Important answers, important questions
- Mosaico and the Future of HIV Vaccines
- Women and Choice: The data say yes!
- Getting PrEP to the People: Lessons in innovation from Kenya and South Africa
- An Evolving Pipeline for HIV prevention
- Cure Research Highlights
- Important Findings on MPox
- COVID-19 and Misinformation
Doxy PEP for STIs, and a vaccine for Gonorrhea: Important answers, important questions
The potential impact of doxycycline (doxy), a long established and inexpensive antibiotic, to prevent a handful of STIs was the subject of several studies.
The DoxyVAC study, presented by Jean-Michel Molina of the University of Paris Cité, (building on a study from last year) had a “DoxyPEP” arm that provided doxycycline to gay men and other to men who have sex with men (MSM) and who were on PrEP and had an STI diagnosis within the last year. These participants took a prescribed dose within 72 hours after condomless sex. Doxy as a post exposure prophylaxis (PEP) significantly reduced cases of syphilis and chlamydia with an incidence of 5.6 percent, compared to 35.4 percent without the intervention. It also reduced incidence of gonorrhea — incidence of 20.5 percent on PEP versus 41.3 percent without it. But Molina warned that gonorrhea develops antibiotic resistance quickly, highlighting the importance of the vaccine arms of this study, which showed that a 2015 vaccine for meningococcal B, a common cause of bacterial meningitis, reduced incidence of gonorrhea from 19.7 percent to 9.8 percent. The results led to an early end to the trial for efficacy, with all participants receiving both interventions. Molina stressed how few options exist today to address gonorrhea, and called for more research. “There’s no safety concern [with the vaccine]. We don’t know how long the protection lasts. We need more data.” AVAC wholeheartedly agrees — an end to the HIV epidemic also means preventing other sexually transmitted infections that can increase risk for HIV and certain cancers and can have other serious consequences. Check out the comprehensive story at aidsmap.com; the recording of last Tuesday’s Margarita Breakfast Club: and certain Moving Forward: Upcoming Strategies on STI Prevention (Recording and Slides); and for more on STI vaccine R & D, go to STIwatch.org.
But DoxyPEP in cisgender women had another story. Jenell Stewart from the University of Washington reported findings from dPEP Kenya, an open-label trial in Kenya among cisgender women who were already adherent to HIV PrEP. Stewart reported that participants had high incidence of STIs at 27 percent, and reported strong but not perfect adherence to DoxyPEP (200 mgs of doxycycline with 72 hours of sex) but there was no reduction in the incidence of syphilis, chlamydia or gonorrhea. Is perfect adherence required; are biological factors at work; or is doxy resistant bacteria the challenge? Stewart called out the urgent need for STI prevention for women and a deeper look at the causes behind these results. For more insight, watch NAM’s Roger Pebody speak with Stewart.
The question of resistance surrounds these findings. There’s international alarm about antimicrobial resistance and the overuse of antibiotics. Research at CROI looked at this issue but did not resolve these questions, with the researchers involved saying much more data is still needed. The momentum behind these findings has brought calls for normative guidance on offering doxyPEP. The Centers for Disease Control (CDC) issued a statement on Monday, February 20 promising to review the data and offering considerations for providers until more detailed guidance is finalized.
Mosaico and the Future of HIV Vaccines
Susan Buchbinder, a leader of the Mosaico Vaccine Trial, the third large-scale trial in recent years to stop early for non-efficacy, released data for the first time showing zero efficacy, as well as an alarmingly high incidence rate in both arms of the study, 4.1 percent. Buchbinder explained in the Monday session of the Margarita Breakfast Club that the Mosaico vaccine relied on prompting non-neutralizing antibodies to work in concert with T-cells to thwart infection.
Buchbinder said “It appears from the series of recent efficacy trials, including Mosaico, that non-neutralizing antibodies are not very useful.” She also said T-cells will continue to be studied as a likely important element in an HIV vaccine alongside neutralizing antibodies.
Mosaico enrolled 3900 cisgender gay men, other MSM and trans women, and offered PrEP at enrollment. Those who wanted PrEP were referred to programs and not enrolled in the study. Those who initially declined PrEP and enrolled in the vaccine arm could opt for PrEP at any point in the study. PrEP use rose over the duration of the study but did not exceed 10 percent of study participants. With all these findings taken together, the study concluded that “despite ongoing risk reduction counseling and linkage to PrEP, HIV incidence…was very high. This is a population in great need of additional effective HIV prevention modalities.” As AVAC has said repeatedly, the Mosaico results highlight why the world still needs a vaccine AND to simultaneously re-double efforts to deliver the prevention options that exist today.
In a special session on the Mosaico results, the head of the HIV Vaccine Trials Network (HVTN), Larry Corey, underscored the message that the field has successfully answered a fundamental question about non-neutralizing antibodies. Corey said they are not a viable strategy for an HIV vaccine, and it’s time to build on the promising results of the AMP studies and continue the development of broadly neutralizing antibodies (bNAbs). “It’s a very rich field, with a rich portfolio.” One key to accelerating that portfolio will be Experimental Medicine Vaccine Trials (EMVT) to quickly identify — and weed out – vaccine candidates. (See AVAC’s May 2022 webinar and resources on EMVTs.) Knowing early which candidates show promise, and which do not, should help the field make better decisions about where to make future investments, in both research and development of next-generation vaccine, antibody and PrEP products and in the delivery of those options that have already been shown to be safe and effective.
Women and Choice: The data say yes!
Despite the sobering news from the dPEP Kenya study, CROI 2023 included lots of good news for women and choice.
Two studies from the Microbicides Trials Network (MTN), found the dapivirine vaginal ring (DVR) to be safe for pregnant and lactating people and their babies. The B-Protected study looked at drug levels in breast milk and was designed to answer questions that would support regulatory authorities and national programs to make the ring available and enable women to make an informed choice. Final results, presented in a late-breaking poster, showed extremely low concentrations of dapivirine detected in infant plasma samples, and that participants used the ring in high numbers. “This favorable safety profile, along with data demonstrating low dapivirine transfer to infants, supports updates to WHO and national guidelines to include breastfeeding people when recommending the DVR as an additional HIV prevention choice,” said Jennifer Balkus, protocol co-chair of the study.
The MTN’s DELIVER study issued similarly favorable interim findings after comparing the ring to oral PrEP during pregnancy. Researchers found dapivirine “posed no safety concerns when used in the third trimester of pregnancy”. The final stage of the study is ongoing and will evaluate safety and acceptability of the ring among people between 12 and 29 weeks of pregnancy. DELIVER is one of very few HIV prevention studies ever conducted in pregnant cisgender women. The risk of acquiring HIV for cisgender women is three times higher during pregnancy. Designing inclusive prevention studies for pregnant and lactating people is imperative; learn more about the issue and advocacy here.
The presentation on the DELIVER study by Katherine Bunge of University of Pittsburgh also called out the role of Good Participatory Practice in robust stakeholder consultations conducted with AVAC in support of the study. For a deep dive on what made these consultations effective check out our blog, Anatomy of Effective Stakeholder Consultation: A look at best practices from a consultation for MTN 042.
Jeanne Marrazzo of University of Alabama at Birmingham School of Medicine reported on data related to PrEP adherence and HIV status. This study pooled data over ten years from 6,296 cisgender women across 11 oral PrEP demonstration projects in six countries. It is the largest assessment to date of real world adherence to PrEP and HIV incidence among cisgender women. The analysis showed 17 percent of 2,954 individuals with adherence data were highly adherent at 7 pills a week. People self-reported higher adherence than researchers objectively measured, but effectiveness was still evident at 4-6 pills per week. This finding offers evidence that cisgender women can have the same peace of mind that men have known for some time: perfect pill taking is not essential. But the data Marrazzo highlighted also points to the need for both more options and innovation in programming. Adherence to PrEP was declining or consistently low for as many as 60 percent of those tracked.
Moses Kamya from the Makerere University, Kampala, Uganda, reported compelling findings from the SEARCH study offering real choices to women who need prevention in rural Uganda and Kenya. In one arm of the study, participants were offered a choice of PrEP or PEP; a choice of access to services at a clinic or off-site; and a choice to use HIV self-testing. The providers working with them were trained in patient-centered care, and these participants were given 24/7 access to a clinician. Kamya reported that “biomedical coverage” increased from 29 percent to 70 percent in the study arm provided with this menu of choices. Self testing went from 34 percent to 59 percent, use of off-site locations went from 22 percent to 61 percent. Kamya said the intervention more than doubled prevention coverage, but this is still far too low for this population. He called for the urgent need to scale up injectable cabotegravir (CAB) for PrEP.
Finally, further analysis of cabotegravir drug levels in women from the HPTN 084 efficacy trial of injectable CAB for PrEP suggest there just might be another win for choice, down the road. Mark Marzinke of Johns Hopkins University presented findings from women in the study who, after dosing every two months as directed by the protocol, experienced delays in dosing for some period of weeks, especially during the early period of COVID-19. Marzinke’s data suggest that doses delayed up to 6 weeks may still provide protection against HIV. Much more data is needed to explore this possibility, but, if confirmed, quarterly injections of CAB for PrEP would align with schedules for injectable contraceptives. Check out the aidsmap story here.
Getting PrEP to the People: Lessons in innovation from Kenya and South Africa
A study in Kenya suggests that trained pharmacists in private pharmacies could be a promising strategy to scale up PrEP, especially among hard-to-reach, unmarried young men. Stephanie Roche of the Fred Hutchinson Cancer Research Center said Kenya’s private pharmacies represent a highly professionalized sector, and the Ministry of Health is seeking evidence to support offering PrEP, PEP and STI testing outside of clinics. The study saw a dramatic increase in demand when fees were waived. Overall, 87 percent of 863 clients used one of the three services, with PrEP uptake at 69 percent. PrEP continuation was 72 percent at month one and 51 percent at month four. Of these participants, 46 percent identified as men and 78 percent were unmarried. A pilot of this study that will offer the ring and CAB for PrEP is under consideration.
Ingrid Bassett of Massachusetts General Hospital presented a study from South Africa that embedded services for PrEP and contraception at three hair salons. Stylists were trained to offer the services. An onsite nurse provided HIV and pregnancy testing, and dispensed PrEP and either oral or injectable contraception. Researchers found very high uptake of contraception, 87 percent. PrEP uptake was 39 percent. Bassett said many of the stylists and clients had never heard of PrEP before. Self assessment of risk was not associated with initiating PrEP, neither was the perception that a partner had other sex partners. But reported intimate partner violence did predict PrEP initiation. Bassett said there was a demand for STI testing as well. This work confirms experiences from the earliest female condom programs in the late 1990s and early 2000s in Zimbabwe which pioneered distribution of female condoms and safer sex information via hair salons — this in turn was built on the mid-1900s delivery of male condoms in barbershops. Clearly, differentiating and simplifying delivery is a concept that can work.
An Evolving Pipeline for HIV Prevention
In 2021, Merck paused treatment and prevention studies using islatravir (ISL) after observing decreased levels of lymphocytes and CD4 T cells, among participants. In 2022, the treatment program re-started, but the prevention studies, testing monthly oral ISL for PrEP, were discontinued. Merck’s Kathleen Squires reported that by 12 months after stopping ISL, lymphocyte and CD4 T cell counts matched the range seen in the control arm, and had returned to normal levels. An examination of a lower dose for treatment showed lymphocyte changes comparable to standard of care antiretroviral therapy. These data along with modeling studies, Squires said, have identified a threshold dose “below which decreases in lymphocyte cell counts are not expected.” While clinical studies for ISL as treatment have resumed, ISL as monthly oral PrEP is “still being looked at” but is not going forward at this time. Merck is looking at alternate drugs that could be delivered on a monthly oral basis.
But ISL could, possibly, be considered as an implant. Squires confirmed that Merck’s ISL implant remains on clinical hold, but a separate research group from Houston Methodist Research Institute presented a small study in macaques that showed a biodegradable implant with ISL offered protection to five out of six animals from a vaginal SHIV infection, with low drug levels detected in the animal with break though infection. Read more on this study here. Of course, animal studies are just the beginning of the process.
Sharon Riddler from the University of Pittsburgh presented data showing that a rectal suppository combining the antiretrovirals tenofovir, alafenamide, and elvitegravir was safe in humans, with high concentrations of drug present in rectal tissue. This suppository is also being tested vaginally. While the injectables and implants often draw the most excitement (and funding), suppositories and other user-initiated, non-systemic products that might deliver protection “right where the action is” could be essential options for people. Researchers called for continued evaluation. Read more on this study and on the potential role for a much wider array of prevention options in this article from Spotlight in South Africa.
Cure Research Highlights
Research presented at CROI 2023 contributed significant evidence that eliminating CCR5, a receptor on T cells that HIV exploits, is a validated approach to control and cure of HIV. Researchers at Emory University provided an update on two trials that used gene editing technology to remove the CCR5 receptor from T cells, making those cells immune to HIV infection. Of the nine participants who had cells modified and went on a treatment interruption, five experienced control for at least one year. One participant remains undetectable six years later, after the single infusion of his own modified T cells. This approach offers a potentially safe and scalable intervention to control HIV without treatment. But questions remain about the quantity of T cells that may need to be altered and if other biological processes are involved in preventing viral rebound.
CROI 2023 also saw the announcement of the Duesseldorf Patient, the third of five individuals cured of HIV through a stem cell transplant. Similar to the other cases, the Duesseldorf Patient received donor cells to treat cancer from a person with a natural immunity to HIV, a mutation that resulted in T cells with no CCR5.
During a plenary on the status of cure research, Janet Siliciano suggested that reducing the size of the reservoir (latent HIV in the body), rather than eliminating it entirely, could be an element in controlling the virus without ART. While approaches to control are making strides, this is one of the questions research still needs to answer.
Just prior to the start of CROI, AVAC joined with a number of partners to convene the 2023 Pre-CROI Community HIV Cure Research Workshop. The 2023 workshop was dedicated to the memory of our friend and colleague Giulio Maria Corbelli, who was instrumental in organizing the first pre-CROI community HIV cure workshop in 2012. The agenda with links to videos of the sessions and downloadable PDFs of slide presentations is available here.
Important Findings on Mpox
A global snapshot on mpox was provided by the CDC’s John Brooks. In 2022, what had been a virus that was mostly isolated to seven countries in west and central Africa spread to 100 countries around the world, resulting in more than 85,000 cases. A new variant of the virus was detected in the majority of these cases and for the first time mpox was highly associated with sexual transmission, primarily among gay, bisexual, and other MSM. Brooks laid out data that showed in some cases people transmitted the virus four days before they developed symptoms. Cases have been declining since August. Brooks points to two possible factors in this decline. A US survey reported approximately 50 percent of respondents took steps to protect themselves by reducing their number of sexual partners. In addition, the CDC has determined that people who received a 2-dose smallpox vaccine were 10 times less likely to become infected. Vigilance against a resurgence must be continued, and randomly controlled trials to validate current treatments must be completed, said Brooks. He also pointed to the heightened severity of mpox among those who are immunosuppressed and the need to prioritize interventions to these populations.
A presentation by Chloe Orkin of Queen Mary University of London drove home these insights. The global case study looked at 382 cases from 19 countries and found the severity of mpox in people living with HIV (PLHIV) who have very low CD4 counts extreme enough to classify it as an AIDS-defining opportunistic infection. A total of 27 people from these cases died. Orkin urged health authorities to add mpox to the 14 other opportunistic conditions that can be lethal to PLHIV who have very low CD4 counts, and for HIV testing for those who test positive for mpox. Get the details on this study from this just published Lancet article. Orkin said it was a matter of equity to get the mpox vaccine more widely distributed: “We must do better.” Stay tuned for a Choice Agenda webinar on March 29 at 9:30 ET that will focus on mpox; Lancet details posted here.
COVID-19 and Misinformation
A symposium on Science Communication in the Age of Misinformation reported on a number of lessons for broader public health and pandemic response. A meta-analysis found that 33 percent of all vaccine information on publicly available social media is misinformation. Another study found almost eight in 10 Americans were uncertain about at least one fact about COVID-19 or the vaccines. Scott Ratzan from City University of New York reported that it’s estimated half of COVID deaths were preventable. Ratzan highlighted a recent study in Nature.com documenting increasing vaccine acceptance in 23 countries including the US, now at 79 percent. Ratzan explored the importance of thinking beyond vaccine hesitancy to understand how fluid opinions and beliefs may be, and he listed a range of trust-building approaches, from early connection with policy makers to long term relationships with communities and greater investment in communication and engagement.
Emily Vraga from the University of Minnesota built on these themes. In addition to debunking bad information, she discussed the idea of prebunking. This includes preparing people to recognize misinformation, identify recycled myths, and call out frequent offenders. Vraga cited Under the Hood of The Debunking Handbook 2020 by Stephan Lewandowsky. Finally, Heidi Larson of the London School of Hygiene and Tropical Medicine and founder of the Vaccine Confidence Project, highlighted issues of identity, belief, grievance, trust and mistrust that fuel the spread of misinformation and strategies to address it. For lots of well-sourced information for your advocacy sign up for AVAC’s weekly NewsDigest and COVID News Brief.
You can delve deeper into all these highlights and more in March when CROI makes these sessions available to the public, and register here for AVAC’s post-CROI webinar, Been There, Did That – Research Reflections from CROI 2023, Thursday March 23rd at 10 am ET. In the coming days and weeks, these scientific advances will help to shape discussions and define action. Watch this space for opportunities to join the conversation.