Developed after hearing from hundreds of stakeholders and scientific advisers, and in collaboration with leadership and staff of NIH’s Institutes, Centers, and Offices (ICOs), the plan is designed to complement the ICOs’ individual strategic plans that are aligned with their congressionally mandated missions [and] will ensure the agency remains well positioned to capitalize on new opportunities for scientific exploration and address new challenges for human health. You can find the NIH strategic wide plan here.
NIH unveils FY2016-2020 Strategic Plan
Human Rights = The End of AIDS
Written by AVAC staffer Micheal Ighodaro, this was first published by the International AIDS Society (IAS).
I was infected with HIV as an adolescent in the streets of Nigeria. As an openly gay man coming from a country like mine, I can tell you first-hand that without addressing human rights we cannot address HIV.
I knew I was gay when I was seven years old. My mum always knew but she always tried to hide it. I remember when I first asked her what the meaning of gay was she told me, “It means evil”. She locked me up in my room for a whole day for asking her what the meaning of gay was. She took me from church to church and to witch doctors who tried to cure me of what she believed I was.
She did this for three years and realized that all she had been doing was not working and that I really was gay. She and my dad hated me so much that my dad asked me to leave the house. I left home when I was seventeen and dropped out of my final year of high school because my dad was not going to pay my fees anymore. I traveled from city to city in Nigeria doing things that I am not really proud of, just so I could get the next meal.
Apart from Bisi Alimi—who was living in the UK and openly gay and HIV positive—no one was openly out as gay and living with HIV in Nigeria because of the stigma and discrimination. I had no idea that I had HIV or that I could contract HIV as a gay man due to lack of information. I lost some of my friends who would still be alive today if it weren’t for the stigma they experienced. It felt like no one was interested in us, gay men living with HIV. It seemed like we were almost left to die. Today, I am really happy for the treatment and prevention that is available now and that many gay men like myself, can live longer and healthier lives.
However, we still have over 79 countries where it is illegal to be gay, bisexual, transgender or intersex. These laws make it almost impossible for us to access HIV prevention and treatment services, which is a direct attack on our basic human rights.
LGBTI populations still face the highest risk of getting HIV in Syria and Afghanistan LGBTI populations face heightened discrimination from ISIS and other religious groups and in most cases are sentenced to death. Many of us are now refugees and asylum seekers in different countries.
As a person who has experienced the discrimination that comes from being gay in my own country, I must ask the question: How far have we gone in protecting the rights of vulnerable populations? This question remains to be answered and goes even beyond the legal rights of LGBTI—it’s about the rights of sex workers, trans diverse persons, people who use drugs, and people living with HIV.
All the recent scientific success we have had in the fight against HIV will come to nothing if we continue to have laws that take away the right of individuals to access life-saving care they need. On this International Human Rights Day, I ask that you stand with me in solidarity for all those who have experienced an attack on their human rights. We should and must do better.
Funding Opportunity: Risk of Adolescence and Injury in HIV Susceptibility (RFA-AI-15-058)
Purpose: To understand how reproductive maturation or injury alters adolescent mucosal environments at HIV susceptible sites in order to provide the safest and most efficacious biomedical prevention strategies (e.g., topical microbicides and Pre-Exposure Prophylaxis (PrEP), etc.). For more information click here.
A December Reading List
It’s the holiday season and in many parts of the world that means lists: of gifts, things to be thankful for, things that are needed and, sometimes, things to read. This week, which began with World AIDS Day, brought more reading material than we can possibly plow through between now and New Year’s Eve. So, in the holiday spirit, here’s a guide to some of the highlights from the new releases and who in your life might enjoy them most.
For the Walk-the-Talk Activist: As described in this post from AVAC’s P-values blog, this week’s International Conference on AIDS and STIs in Africa (ICASA) in Zimbabwe has brought bold advocacy and activism from women’s groups, sex workers, gay men and other men who have sex with men, trans-diverse people, women living with HIV and many other groups. Unfortunately, there have also been rights violations and harassment of people, including many individuals from “key populations”. Our blog provides first-hand accounts and info on how UNAIDS responded.
For Anyone with a “Wonder Woman” in their Lives: An AVAC blog on the new Innovation Challenge for the DREAMS Initiative, a program aimed at adolescent girls and young women. The Innovation Fund is designed to infuse additional money into bold programs—and bring in new private-sector partners.
For the Implementation Advocate (who can live without photo captions): The new World Health Organization policy brief on what’s new in the second edition of the Consolidated Guidelines on the Use of Antiretrovirals (ARVs). If you feel like you’ve missed the second edition (the first, issued in 2013, can be found here), fear not. The full guideline still isn’t out—WHO has said to watch for it in 2016. But this policy brief gives important highlights and expands on the early release guideline on PrEP and when to start ART, which came out in September.
The newest document highlights what’s truly new. In the ART section, WHO, for the first time, advances a “differentiated care” approach that sees people living with HIV in categories other than CD4 cell count, and pregnant or not. The document begins to map what it would take to deliver services in a world where people who are unstable on ART receive one type of intervention, those who are healthy and newly diagnosed, and so on. It won’t be easy—but it wouldn’t be possible without this type of detail.
If you’re looking for captioned photos, this is a document to avoid: pictures of people apparently from low- and middle-income countries abound, but with no identifiers, and it’s hard to tell when, where or why the pictures were taken. In a document that recommends looking closely at each individual and his or her reality, the illustrations would be a great place to start.
For the Two-Briefs-Are-Always-Better-Than-One Advocate and the PrEP-Curious Reader: A two-page policy brief on PrEP from WHO that’s short and to-the-point. This is a great handout to show to people who want just the facts on why WHO now states “#offerprep” as a strong recommendation.
For the Number Cruncher (who likes photo captions): Volume Four of the One Campaign’s “Unfinished Business” report on global financing for HIV manages to be both clear, simple and comprehensive about who is spending what—at the country level and in the private sector. It also features country-specific pages and recommendations, trend analyses and clear advocacy “asks” for the Global Fund, African countries—and more. Fans of captions will be happy to see that every picture has an explanation of who is shown, where they are from and what they do.
For the Unsatisfied Realist: Treatment on Demand for All, a policy analysis paper by Health GAP and partners that maps the gaps between policy and reality when it comes to ART access worldwide. Noting that fewer than 1 out of 10 people living with HIV worldwide live in a country where immediate ART (as recommended by the WHO) is current policy, the report describes the state of, and remedies for, this great global divide.
For the Precision-Minded PrEPster: The full New England Journal of Medicine article presenting the findings from the IPERGAY trial that evaluated “on-demand” PrEP in gay men in France and Canada. Steer clear of the press release and subsequent media which suggests that the study found evidence that coitally-related dosing is effective and head straight for the discussion section which clearly states that the only conclusion IPERGAY can draw is that four pills per week provides high levels of protection in this study population.
Evaluation of the levels of drug needed to provide protection in the context of anal sex back up this conclusion—which, for now, is clear evidence that a daily PrEP regimen can be forgiving of a few missed doses for gay men and transwomen. Now is not the time to shift from the message that a pill a day provides protection. For more on PrEP’s pipeline and interpretation of the IPERGAY results, check out the two articles in POZ magazine.
Pour les Francais et leurs Amis: For the French and those who love them, lift a glass for resilience in the face of terror and another for the announcement from French Minister of Health, Marisol Touraine that will bring government-subsidized PrEP to those who need and want it.
For the Speed Readers: Ending the HIV-AIDS Pandemic—Follow the Science, an editorial in the New England Journal of Medicine. In it, Anthony Fauci and Hilary Marston of the US NIH need just over 1,000 words to summarize the science that has defined progress in the epidemic.
Happy reading—and let us know what’s on your list!
Outright Activism as ICASA 2015 Starts with Violations and Silence on Key Populations
Many activists arriving at the airport in Harare, Zimbabwe for the International Conference on AIDS and STIs in Africa (ICASA) saw familiar faces, greeted far-flung comrades and headed for the passport desk and baggage claim expecting this meeting to be like others in the past—a chance to share strategy, recharge and set priorities for the coming year in dialogues led by and for Africans and their allies.
Instead, even before exiting the airport, things took an unexpected turn: sex workers, gay men and transgender women and even activists who just “looked different” reported having materials confiscated, being personally detained, having their passports held and being charged duties to reclaim their posters and educational materials.
At the conference venue, trouble continued. UNAIDS head Michel Sidibé opened the conference with remarks that, while stirring, made no mention of “key populations”, including gay men and other MSM, transwomen, sex workers and others. This prompted a sign-on statement asking Dr. Sidibé to “Walk the Talk”, of the messages of support he gives these groups behind closed doors.
Dr. Sidibé and UNAIDS listened, and when he officially opened the Community Village on November 30th, he said, “Key populations are helping us to break the conspiracy of silence.” The full statement UNAIDS made on this issue can be read here.
Unfortunately, discrimination and challenges have continued at the very gathering that should, and indeed must, be a safe space for everyone working on HIV. Here are some additional voices from the frontlines:
Micheal Ighodaro (AVAC): Coming here I was expecting [ICASA] to be the standard it was before. At the ICASA conference in Addis, we were allowed to come and go freely. Here, materials were detained and MSM and transgender people were questioned regarding the content of their materials. My materials were detained at the airport for the Key Populations Preconference. While that issue has been resolved, ICASA organizers did not apologize at the opening for what everyone has had to go through simply to get their materials to the conference. I thought most ICASA organizers would have known better.
Regarding key populations at the conference, people weren’t sure it would be safe to attend. People are more scared after all that they are seeing. I met some friends following a day of sessions and the restaurant made an announcement soon after we’d arrived stating, “No more sex workers here.” No one I was with was holding hands or doing anything to attract attention. I’m more concerned and angry, I was expecting to see better both at ICASA and in the country. We tried to have t-shirts printed with #WalktheTalk; however, the printer here in Harare refused to print them since some of the designs include “MSM” and “sex worker” on them.
Carolyn Njoroge (Kenya Alliance of Sex Workers): On arrival to Harare there was a lot of screening and questions, asking what we came to do, if we were coming for ICASA as part of a group. They opened our bags and everything we had that included the words, “sex worker”, including my poster presentation on advocating for rollout of PrEP for male and female sex workers, our t-shirts and all other materials, was confiscated. Additionally, three transgender people were locked in a room and their passports were taken away. We reached out to the African coordinator for ICASA and they were eventually released.
We were told that the laws in Zimbabwe do not allow that sex work can be practiced—according to “regulations and morals”. All our materials were left at the airport and we had to pay to get them released. They were finally released this morning [Monday], after originally being told we could not bring them into the country but could only get them on our way out of the country.
When we got here this morning, the conference organizers had removed everything that said “sex workers” from our booth in the Community Village and told us we had to call ourselves, “Key Population S” and “Key Population M” [for MSM]. After we said no, they decided we did not need to do this, but did move us to the back tent. [The Village is a series of three tents connected through small walkways. The Sex Worker Zone and MSM Zone are in the last tent].
At the hotel, we gave our passports when checking in and I was asked what I had come to do. I told them I was with ICASA, and they asked with whom. I told them I was supported by the African Sex Workers Alliance and am a sex worker from Kenya. They told me the hotel had regulations—no wearing of miniskirts and shorts past 6:00 pm, no looking at people like you want to solicit, no wearing indecent clothes, we can’t go out late and come back late. When we booked at the hotel they saw who we are affiliated with, why did they agree to let us stay there?
Police arrested a male sex worker at the Sex Worker Zone booth. The officer was not wearing a uniform and came in with the purpose of getting a sex worker to agree to sex. We are scared and trying to travel together to and from the conference, or stay in our hotel rooms.
If the government of Zimbabwe agreed to host ICASA, they knew it would bring people from diverse populations. Why did they agree to host?
What can you do?
- Become an ally to LGBT and sex worker groups in your country—contact AVAC for more information.
- Email anyone you know at ICASA asking them to call on speakers to state, in their opening remarks: “I stand in solidarity with African key populations: sex workers, men who have sex with men, trans diverse persons, people who use drugs and all people living with HIV. Protecting their rights is essential to the fight to end AIDS.” (This statement was developed by civil society groups representing key populations.)
New Funding for DREAMS, New Targets for Advocacy
World AIDS Day brought a flood of announcements—and for advocates who’ve been following the DREAMS initiative—a joint venture of PEPFAR, the Bill & Melinda Gates Foundation and Girl Effect (the Nike Foundation)—there was news of note.
Speaking at the International Conference on AIDS and STIs in Africa (ICASA), in Harare, Zimbabwe, Ambassador Deborah Birx, head of the PEPFAR program, announced the details of an “Innovation Challenge” fund that would bring new money and new partners to the initiative, which is focused on bringing down rates of HIV in adolescent girls and young women.
Ambassador Birx announced that the DREAMS Innovation Fund would combine US$80 million in PEPFAR funds (a new allocation from within the existing budget) with US$25 million from new private sector partners Johnson and Johnson and ViiV, as well as support from Gilead, with a specific focus on providing PrEP as part of the DREAMS country plans.
The precise plans for how the Innovation Funds will be disbursed, including timelines for applications to the fund, framing of the requests for proposals, and so on haven’t been revealed yet. A fact sheet on the Innovation Challenge can be found here.
The next step for advocates? Keeping up the pressure on OGAC and PEPFAR country offices to ensure that civil society coalitions are engaged in both Innovation Challenge planning and overall DREAMS implementation. With dialogues happening right now at ICASA on this very topic (follow @hivpxresearch for the latest), this is already in the works. Not in Harare? Be in touch to get involved.
AVAC on World AIDS Day: We’re 20. We’re not giving up.
When AVAC was founded in 1995, we were called the AIDS Vaccine Advocacy Coalition. Our singular goal was to advance swift, ethical research for a vaccine that was then — and is today — essential to bring the epidemic to a conclusive end.
Twenty years later, AVAC is still focused on swift and ethical research, but our scope has expanded. Along with vaccines, we advocate for PrEP, microbicides, voluntary medical male circumcision and more.
Through it all, our message has been the same: prevention is the center of the AIDS response. Not just any prevention but smart, evidence-based, community-owned, rights-based strategies.
We do this work because it’s essential. We are able to do it because of our robust partnerships worldwide. We will keep doing it — with your help — until the epidemic has, finally, come to an end.
 We’ve experienced 20 years of breakthroughs and disappointments in prevention research. A vaccine that many had given up on was the first to provide modest protection. One microbicide everyone hoped for didn’t pan out. Male circumcision and PrEP studies overcame skepticism and, together with antiretroviral therapy, paved the way for a prevention revolution.
We’ve experienced 20 years of breakthroughs and disappointments in prevention research. A vaccine that many had given up on was the first to provide modest protection. One microbicide everyone hoped for didn’t pan out. Male circumcision and PrEP studies overcame skepticism and, together with antiretroviral therapy, paved the way for a prevention revolution.
Through it all, AVAC has worked with partners to maintain the field’s focus and press for continued research into an AIDS vaccine, a cure and more.

 When AVAC was founded, the only biomedical HIV prevention options for adults were male and female condoms. The pathway for introducing any new strategy was largely unmapped. No one knew where the gaps would be—between trial result and country action, between guidance and financial support. Now we do.
When AVAC was founded, the only biomedical HIV prevention options for adults were male and female condoms. The pathway for introducing any new strategy was largely unmapped. No one knew where the gaps would be—between trial result and country action, between guidance and financial support. Now we do.
Over two decades, AVAC has not only identified the gaps; we’ve worked to bridge them, so that products reach people in programs that work — without delay.

 Twenty years ago, advocacy for HIV prevention hardly existed. So AVAC helped build a global network of advocates equipped with effective advocacy strategies and the latest evidence.
Twenty years ago, advocacy for HIV prevention hardly existed. So AVAC helped build a global network of advocates equipped with effective advocacy strategies and the latest evidence.
With our support, they are putting prevention on the agenda in countries and communities around the globe.
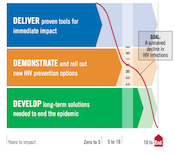 When the world lacked a plan for ending AIDS, we helped create one.
When the world lacked a plan for ending AIDS, we helped create one.
Now we’re holding global leaders accountable for results — demanding the resources, policies and evidence-based plans needed to deliver all of today’s prevention options to the people who need them, and to plan for the rapid rollout of new options as they emerge.

 Communities’ support for prevention research can never be taken for granted — it has to be earned. For 20 years, we’ve helped build trust between researchers, funders and communities to speed the ethical development and rollout of new prevention options.
Communities’ support for prevention research can never be taken for granted — it has to be earned. For 20 years, we’ve helped build trust between researchers, funders and communities to speed the ethical development and rollout of new prevention options.
And when controversy threatened to derail those efforts, AVAC provided leadership and resources to help get them back on track.
Your gift to AVAC will support our efforts to accelerate the development and delivery of HIV prevention options to men and women worldwide. With your help, we can continue to convene, collaborate and communicate a strong, clear and cohesive vision for HIV prevention today, tomorrow and to end the epidemic.
It will take all of us working together to end AIDS. Please join us.
Give Us the 2-in-1 HIV Prophylaxis
In this Mail and Guardian editorial, South African advocates call on the South African government and health department to do its part to expand the provision of PrEP and integrate it into combination treatment and prevention programs before “people are agitated and take to the streets to demand these tools”.
South Africa has rolled out the largest antiretroviral treatment program in the world—about 3.1 million people are now on treatment, according to health department figures.
This is a remarkable, given the earlier years of poor political response. But South Africa still has unacceptably high rates of infections and HIV remains a public health emergency.
Within the general epidemic in South Africa, some specific population groups—such as sex workers, gay men and other men who have sex with men (MSM), discordant couples (where one partner is HIV-positive and one HIV-negative), truckers and people who inject drugs—have higher rates of HIV and require specialised interventions.
The disease takes a particularly devastating toll on the lives of adolescent girls and young women between the ages of 15 and 24, a rate more than four times that of their male counterparts, according to the Human Sciences Research Council’s 2012 National HIV Prevalence, Incidence and Behaviour Survey.
The HSRC survey, also found that more than 400,000 new HIV infections occurred in 2012, bringing the number of people infected in South Africa to 6.8 million in 2014.
A disturbing picture
These statistics present a disturbing picture of the HIV epidemic and our response. In delaying the implementation of pre-exposure prophylaxis (PrEP), has South Africa failed to embrace the wisdom of science?
This new option for HIV-negative people at substantial risk of HIV infection is a combination antiretroviral drug, TDF/FTC, taken once a day, which can drastically reduce their chances of becoming infected. Research studies show that, when this two-in-one pill is taken correctly and consistently, it is more than 90 percent effective.
There have been unexplained delays by the Medicine Control Council to approve and license TDF/FTC as pre-exposure prophylaxis and the department of health’s response to South Africans voicing their demand for this action has been silence. The council should approve TDF/FTC before the end of this year.
New guidelines
Advocates welcomed the World Health Organisation’s (WHO) new guidelines for HIV treatment, released in September. These recommend that: “Oral PrEP… should be offered as an additional prevention choice for people at substantial risk of HIV infection as part of combination HIV prevention approaches”.
The new guidelines have broken the silence among policymakers on the future of pre-exposure prophylaxis in South Africa. Following their release, Yogan Pillay, the health department’s deputy director-general for HIV, endorsed the WHO guidelines in an article in the Mail & Guardian. This demonstration of commitment is an important step in realising our dreams about providing pre-exposure prophylaxis.
As HIV prevention advocates, we talk to many people, including potential users of TDF/FTC. We hear from a host of people from all walks of life who are demanding pre-exposure prophylaxis. They want to know when the drug will be available in South Africa and how they can get access to it. These questions have been previously been impossible to answer, but now we hope to work with health department. Will the department follow through on its commitment and the ethical imperative to provide medicine that is a crucial step in confronting the HIV epidemic?
We would like to see such a programme rolled out in the shortest possible time, and through existing structures, where possible.
We know that implementation of this new intervention will not be easy. It requires political will, dedicated advocacy, domestic sources of funding and international donor commitment.
More importantly, investment must be based on decisions that are driven by evidence rather than sentiment. The health department will need support from a variety of stakeholders—much of which can and will come from the huge groundswell of civil society support for the implementation of a pre-exposure prophylaxis programme.
Timeline
As we prepare to support the department in planning and executing such a roll-out, we have questions. What are the department’s plans for this? What are the timelines? Has the department started seriously with advocates in the provinces? What are the advocacy issues that civil society can push?
We need effective models to deliver PrEP. Demonstration or pilot projects in South Africa and around the world will provide us with the knowledge to guide a roll-out in real-world settings. The health department can also take advantage of data on existing public health programmes that can be adapted for providing TDF/FTC.
Some organisations that already provide comprehensive HIV prevention services are suggesting that the department use existing structures and services to start and expand the provision of PrEP and integrate it into combination treatment and prevention programs.
Within these organisations, there are champions who have already established positive working relationships in communities. They can help to identify barriers to implementing and recommend strategies to address the barriers.
Recommendations
Young women tell us, “We recommend that youth-friendly clinics be established and that health staff be sensitised about the unique needs and problems that young people face.” Similarly, sex workers have suggested that TDF/FTC should be provided “within user-sensitised facilities” and, where possible, through mobile clinics. Men who have sex with men are calling for the medicine and some are already getting it from private clinicians through “off label” prescriptions.
As advocates, we will continue our work to educate the public about TDF/FTC, how to get it and how it can further strengthen existing HIV prevention efforts. But we know that there is more to be done through working closely with people and with social marketers.
We will also continue preparing for the results of a vaginal microbicide ring study expected early next year. The vaginal ring, another form of PrEP, slowly releases the antiretroviral drug dapivirine over the course of a month. If proven safe and effective, the vaginal ring could expand options for women-initiated HIV prevention methods.
Civil society is working with the International Partnership for Microbicides, the organisation which developed this technology, and other partners who conducted microbicide research among South Africans to plan for the results and introduce the product if it is proven effective. No microbicide has yet been licensed for use.
We acknowledge South Africa’s remarkable success in fighting HIV. There is now opportunity to build on these successes by taking advantage of new innovations such as TDF/FTC to reduce the chance of infections and save on treatment costs. HIV-negative South Africans have a right to use this life-saving intervention now.
We should not have to wait until people are agitated and take to the streets to demand these tools.
Will South Africa show global leadership and take immediate action to get PrEP into people’s hands? Or will our collective conscience be haunted in years to come, knowing we could have averted new infections and saved on costs of lifetime HIV treatment and sickness? The science is clear that TDF/FTC works when taken correctly and consistently; now we must follow this evidence and act on it.
John Mutsambi is an AVAC Fellow. AVAC is a US based organisation that advocates for HIV prevention to end AIDS. Brian Kanyemba, Yvette Raphael and Ntando Yola are the leaders in PrEP advocacy in South Africa.
ICASA 2015: A conference guide to participating on-site and virtually
For the latest from the conference, visit our ICASA page.
This update includes information on the 18th International Conference on AIDS and STIs in Africa (ICASA 2015). Featured below are details on select events related to biomedical HIV prevention research and implementation as well as how to follow the conference from afar.
The 18th ICASA conference theme is AIDS in Post 2015 Era: Linking Leadership, Science & Human Rights. AVAC and many of our partners will be participating in and presenting at the conference. There are several ways you can link to HIV prevention research and rollout-related events—both in-person and from afar:
- ICASA 2015 HIV Prevention Research Roadmap: There is a wide range of sessions planned for the conference (full program available here), and we have pulled together a roadmap of select sessions that may be of interest to those tracking biomedical prevention research and rollout. Download as a PDF or XLS file and please let us know of any other related events that should be added to the roadmap.
- Biomedical HIV Prevention Forum (BHPF) Pre-conference Session: Hosted by the New HIV Vaccine and Microbicide Advocacy Society (NHVMAS), in collaboration with a number of partners including AVAC, this session will take place on 29 November from 9:00 to 16:00 at the Rainbow Towers. See the BHPF website for more information.
- Key Population Pre-conference Session: Hosted by African Men for Sexual and Health Rights (AMSHeR), African Sex Workers Alliance (ASWA) and Gender DynamiX, this session will take place on 28 November and 29 November from 9:00 to 17:00 each day at the Crowne Plaza Hotel. For more information contact [email protected].
- Youth Pre-conference Session: Hosted by the ICASA YouthFront, this session will take place from 27 November to 28 November from 9:00 to 16:00 at the Rainbow Towers. For more information visit the YouthFront website.
- Satellite Session: Adapting the WHO guidelines on oral PrEP: What will it take?, hosted by USAID, PEPFAR, WHO and the OPTIONS Consortium, comprised of FHI360, Wits RHI and AVAC, this satellite session will take place on 3 December from 7:00 to 8:30 at the Rainbow Towers. The panel will cover an overview of the WHO Interim Guidelines and key oral PrEP research findings and demonstration projects, with a discussion to follow on what it will take to introduce and scale up PrEP and other ARV-based prevention options within combination prevention programmes. Breakfast will be provided. For more information contact us.
- WNZ@ICASA: AVAC is excited to partner with many African partners on sessions at the Women’s Networking Zone (WNZ) at ICASA. Please check out the WNZ programme and please visit the zone for opportunities to engage and dialogue with women’s organizations across Africa. AVAC is collaborating on a number of sessions and dialogues at the WNZ, including session updates on the dapivirine ring trials, PrEP for women, hormonal contraception and HIV, women’s role in VMMC rollout, barriers in access to treatment and HIV prevention research and delivery.
ICASA on Social Media: Follow the conference in real-time on social media by following us on Twitter and Facebook — and using the official conference hashtag #ICASA2015.
Want a Healthy World? Let the HIV Response Lead the Way
This post first appeared on The Huffington Post.
World AIDS Day 2015 comes at a watershed moment in the fight for the health of people living with HIV and for the health of all the citizens of this planet. The two are intimately related: HIV has, for the last three decades, defined the landscape of ambitious, collaborative and innovative responses that marry science, rights, community-based responses and structural change. Ultimately, these responses can be leveraged to improve health everywhere, but only if we continue to make real progress in battling HIV.
In recent years, collaborations between research teams and thousands of volunteers in clinical trials have yielded insights into how to use HIV prevention and treatment options to end the epidemic. These insights have led to the Joint United Nations Programme on HIV/AIDS (UNAIDS) “Fast-Track” approach to ending the epidemic, which sets ambitious targets for a range of interventions, including 27 million voluntary medical male circumcisions by year 2020, three million people on daily oral pre-exposure prophylaxis (PrEP) annually, major reductions in violence against women, improvements of human rights and, of course, the 90-90-90 targets for 2020: 90 percent of all people living with HIV will know their HIV status, 90 percent of all people with diagnosed HIV infection will receive sustained antiretroviral therapy (ART) and 90 percent of all people receiving ART will have viral suppression.
The world has gotten this far because of massive investments in the HIV response. To actually end the epidemic, though, it is imperative that we resist complacency, cutbacks in funding and a sense that, on any level, our work is done.
Over the last 15 years, the Millennium Development Goals guided the global response to development. Health, including controlling HIV, figured prominently in these goals. In September, the members of the United Nations adopted the Sustainable Development Goals (SDGs), which will guide policy and funding for ending poverty everywhere over the next 15 years. Health is one of 17 goals. To meet it, funders, implementers and country governments will need to be smarter with investments in HIV/AIDS. This means working side by side with people living with and most affected by HIV to develop rights-based approaches and efficient and community-supported service delivery models. And, it means thinking beyond any single health issue and toward integrated approaches that both fight HIV and contribute to ending poverty, hunger and inequality.
This integrated, rights-based approach is needed for all the SDGs. But just as HIV has transformed the way that the world thinks and acts on a single issue, it must also be the leading edge of the pursuit of even more ambitious targets: end epidemic rates of new HIV cases, but also begin to change the quality of life for people everywhere.
Is this a lot to ask of the response to a single virus? Perhaps. But HIV is a virus that reveals the fault lines of societies. HIV follows poverty, stigma, discrimination, criminalization and inequity. Treating HIV effectively means addressing these issues. In many parts of the world, girls and young women are at particular risk, as are men who have sex with men, transgender individuals, sex workers and people who inject drugs. A human-rights-based approach that engages these key affected populations is the basis for a sound, effective response.
Successful achievement of both the SDG health goal and the UNAIDS Fast-Track targets hinges on innovation. Here, too, the HIV response lays tracks for the path to true global change. Over the last few years, the HIV prevention, care and treatment cascade has emerged as an effective tool for describing the status of the response, influencing policymakers and guiding investments in treatment and prevention. Consistent use of effective ART both improves the lives of those living with HIV and dramatically reduces the chance of transmitting the virus to others. New World Health Organization (WHO) guidelines recommend that people with HIV start ART regardless of their stage of infection. WHO also provided a huge step forward for daily oral PrEP by recommending this proven intervention for all people at substantial risk of HIV infection. More recently, UNAIDS included PrEP in its prevention targets, while the US President’s Emergency Plan for AIDS Relief (PEPFAR) Scientific Advisory Board just released a strong recommendation for PrEP.
Delivering daily medications to both HIV-positive and HIV-negative people in programs that are supportive, accessible and sustainable is a major challenge. But, it can be done. And if it can be done for HIV, it can be done for many other strategies, too. Today’s HIV investments are increasingly focused on creating platforms for health delivery as part of a comprehensive approach to women’s sexual and reproductive health.
Happily, these investments will not only increase the impact that existing interventions can have today, but will also lay the groundwork for eagerly anticipated ARV-based microbicides, especially the vaginal ring with dapivirine, if and when it is demonstrated to be efficacious in clinical trials that will report out early next year.
While the range of options for impacting HIV has grown tremendously, additional research is needed to make things simpler to use, to expand choices and to make health a reality for all. Here, too, HIV is aligned with the broader health response, which seeks to expand access to effective vaccines and durable cures to a range of other diseases. We believe the same tools—a vaccine and a cure—can and must be pursued for HIV.
The broader goals of the SDG era will likely see increased attention on integrated programs that combine multiple health programs, rather than disease-specific programs, with links to education and social and economic development efforts. Smart investments to sustain the momentum for HIV/AIDS control will strengthen health systems and contribute greatly to ending poverty, hunger and inequality, moving the world closer to ending HIV/AIDS once and for all.


