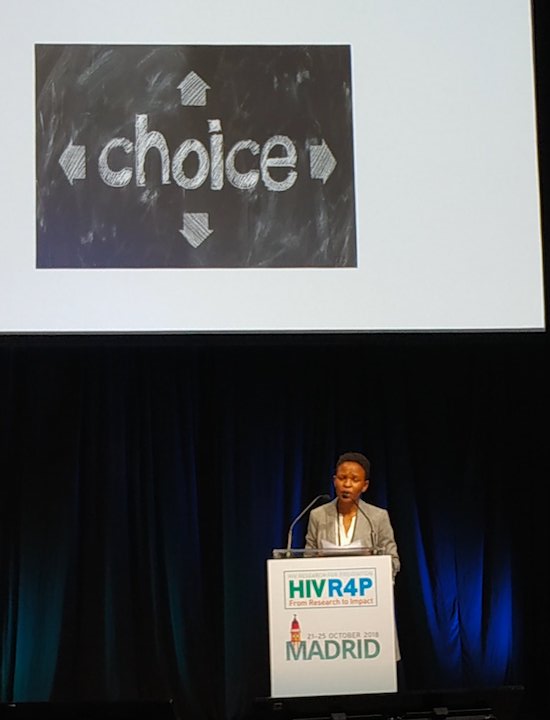
AVAC’s Maureen Luba gave this essential plenary talk on a multipurpose prevention revolution at the HIV Research for Prevention 2018 conference, held in Madrid, Spain. Affectionately known as R4P, it’s a space where HIV prevention takes center stage. Read Maureen’s remarks below or watch her presentation here.
This last Sunday morning I got a very disturbing WhatsApp message from one of my closest friends and the message read:
“Good Morning Maureen, I just found out that my husband is having an affair with someone who is HIV positive. I don’t know what to do and Maureen you know I can’t leave him but my only challenge is that he hates condoms. When are you coming back? I really want to talk to you!!!
I felt helpless, I felt hopeless, and I asked myself some really hard questions: am I doing enough work as an advocate? Is the work that I have been doing really making an impact and is it really worth it? How can I call myself an HIV prevention advocate when I can’t even advise my own friend how she can protect herself from getting infected simply because her husband hates the condom and which is the only HIV prevention available for her (since we still don’t have PrEP in Malawi and we don’t know we are going to have it and I don’t even know if it was available she would like it).
Well you can imagine how painful this week has been for me. When I was coming to this conference for me it was just one of those, but when I got this message it gave me the impetus as to why I needed to attend the conference this week.
I know we all wear multiple hats and affiliations, but whether we are advocates, researchers, funders or policy makers, we are all part of communities, families and relationships. So I speak today as one Malawian woman wearing all my hats proudly.
For me a multi-disciplinary prevention revolution which is the title of my presentation is about four things. It is about a comprehensive, concerted, integrated and sustained response!!!
Comprehensive
And by comprehensive what I mean is that:
- We need to we design, develop and implement a wide range of products, programs and interventions that takes into consideration the different needs and vulnerabilities of different populations.
- It’s not about either/or.
- It is about providing a wide range of choices so that people like my friend can be able to choose the product that meet her needs.
- On Monday this week, my colleagues and comrades stood on this stage with banners written Choice All Over and Jim Pickett (whose persistent I admire so much) and that amazing young doctor from Tanzania passionately reminded us all why choice is important!!
- And I just wanted to use this moment to reinforce their call and that many others at this conference had made – we are not going to end this epidemic if we are not giving people choices!
- We are all working on the same side.
- And we are all working for the same goal. It is not about shame or blame.
- And fighting should not be the only way for us a reach a consensus!!
- We can do this better.
- When I was doing my AVAC Advocacy Fellowship in 2016, immediately after the ASPIRE and Ring results were announced at CROI, a few women from my community reached out to me and asked me where they could access the ring.
- For them the 31 efficacy did not mean as long there was some level of efficacy in it.
- To them they felt the ring could be able to meet their needs.
- And the ring is just one example.
- HIV prevention can become more comprehensive if we all understand and accept that that we can’t sacrifice good enough simply because we are in search for perfect.
- Because, ironically, the thing we are calling imperfect may be good enough for many people who want and need it.
- The voices we raise are not about making choices between long acting versus short acting.
- But it’s about what works for different people.
- Hence it’s not about having one clinical trial at a time, but rather it’s about multiple, simultaneous trials that are able to address the urgent needs of different people.
- Comprehensive prevention also means delivering the options available now whilst developing options we need for the future.
- The tools that exist today need to be implemented, not only because they have levels of protection but because they form the platforms for future strategies.
- Today’s daily oral PrEP program is tomorrow’s PrEP + ring + structural intervention platform.
- And tomorrow’s dapivirine ring program is the platform for a revolutionary integration of HIV and family planning via multipurpose prevention tools.
Concerted
On the other hand, a concerted prevention revolution means controlling or ending the epidemic will require concerted efforts from different stakeholders including from policy makers, funders, CSOs, advocates, communities and the end users.
- Experience has shown us that when funding decisions are made in concert with all relevant stakeholders, the impact is way more better than when it is not only a single entity weaving the influential narrative of what gets funded and what does not.
- We need to create a space where everyone’s needs, fears, vulnerabilities are inherently valued and accorded the desired attention!
- To our funders, we know sometimes it’s really hard to choose from all these competing priorities, but together we can make those hard decisions and achieve the desired impact in the end!!!
- All we need is to recognise the expertise each one of us brings to this discussion and supporting each other’s efforts so that, synergistically, we can be able to enhance the impact of the individual spaces which we occupy.
- Again, it is about having one research agenda that is co-created by researchers, policy makers, funders, communities and end users.
- Like I said, all of us have the same goal which is to the end the epidemic.
- Yet currently everyone seem to be serving their own agenda.
- Advocates: we do have our research agenda, principal investigators have their own research agenda too and so do policy makers and funders!!
- Yet we know that the only way we can end the epidemic is by co-creating an agenda that prioritizes the needs of those affected by the epidemic.
- Talking about a co-created agenda, on August 30th this year (almost two months ago), civil society in Malawi conducted a national research consultation meeting where we brought together site investigators, ethics research committee representatives, policy makers and development partners in our room to discuss some of the critical issues in research in Malawi.
- This was a meeting organized and funded by civil society, with civil society leading the agenda setting with input from everyone else.
- One of the agenda items for the meeting was a discussion on the National Health Research Agenda (a document which highlights research priorities in Malawi).
- Everyone in the room had a chance to contribute to what should be included in the research agenda.
- I tell you this meeting was such thing of a beauty!!
- Everyone loved it!!!!
- I remember one of the principal investigators saying ‘Can we have such type of meetings every 6 months?’.
- And this just demonstrates the ability for us to co-create only if we choose too.
- It is possible if we make it happen.
Integrated
Integrated prevention revolution on the other hand is not requiring programs or stakeholders to lose their primary focus.
Rather, it’s about figuring out how do all these interventions that we are designing, implementing and advocating for fit into the broader context and complexities of the target populations.
- When we know that increasing frequency of clinic visits does not fit into the realities of the lives of women.
- Hence, when we are developing products and designing programs, we need to be being conscious of the fact that the same women we are targeting for our PrEP programs are the same women with two monthly clinic visits for DMPA shot who could also be same target population for once monthly bNAb vaccine shots.
- When designing our research and implementation programs, we need to design studies that recognize, recruit and follow up study participants as social beings and not just a biological product.
- Trials can only do better by paying enough attention to what is happening on the ground.
- Which many of us may have been missing — not by a purposeful act of omission — but maybe it’s because we simply don’t know how to reach and interact with communities as social beings!
- Well that’s our function. As your partner – as community advocates, we are here to support you and provide those insights.
- We can help bridge that gap.
- And we are very passionate about making things work.
- We have made HIV work, as history will recount.
- We have made research work for treatment.
- We created the concept of microbicides for our needs.
- We have pushed the field this far.
- We can push further whatever it is we co-create.
- We are alive to transparency and accountability.
- As watchdogs, this is the role we have to play.
- As different stakeholders we all have different strengths.
- But with synergy, we can achieve a lot more with our individual strengths.
- The lines in the HIV field are becoming blurred.
- The silos are breaking.
- With waning resources in the terrain, working synergistically is the only way we will all achieve our goals cost effectively.
- We do not need to learn lessons after huge expensive trials.
- There are lots lessons we can learn by listening, hearing, trusting and doing.
- I am an example of how we advocates drive the field with passion.
- I am an advocate from Malawi.
- I am a key player in the civil society space.
- I am a member of the Vaccine Advocacy Resources Group on whose platform I advocate for vaccine research.
- I am also a Board Member for Intentional Partnership for Microbicides where I have been strongly advocating for microbicides and the HIV prevention needs of young women.
- Back home I sit on the PrEP task force where I work with my CSO colleagues to advocate for the roll out of PrEP.
- I am also one of the core group members for AfnHI where I have been advocating for increased regional and sub-regional funding for HIV prevention.
- The list goes on.
- To some of you may, this may read like a confused human being.
- I however reflect the lives of many advocates seated in this room who think about integration rather than silos.
Sustained
Lastly it is about a sustained response and by this I mean:
- HIV prevention can be sustained if countries and communities are able to own the response.
- It’s about governments beginning to own the response.
- We as community members are leading that push for government ownership.
- We push for regulatory actions now ahead of the future.
- We advocate for country preparedness for future products down the line.
- Because we believe we are the face of the sustained interest in biomedical HIV prevention research.
Closing
In closing!!!
- It’s has been great conference for me, but sadly as am going back home to my friend and I am still not sure how I am going to help her.
- I still don’t have the right answers for her!
- And she is just one of millions people across the globe who are in similar situations like her.
- I hope by the time we will all be leaving this conference today everyone of us in this room will realize that the stakes are high.
- We need to build bridges between science and real life experiences, responses need to be comprehensive, approaches have to be integrated and our efforts need to be sustained.
- There is no time for complacency.
Thank you!!!!