Rob Newells is the newly appointed Executive Director of AIDS Project of the East Bay; he is minister and founder of the the HIV program at Imani Community Church in Oakland and is a PxROAR member since 2012.
The annual Conference on Retroviruses and Opportunistic Infections (CROI) brings together thousands of researchers from around the world to share the latest information on HIV, AIDS, and related infectious diseases. The 2018 meeting in Boston highlighted 114 oral abstracts and 991 posters in 23 different science categories, from Virology to Population and Cost Modeling.
The time lag from research to implementation in health can be long. One study from 2011 suggested an average 17-year delay (Morris, Wooding, and Grant, 2011). This graphic (adapted by AVAC from Dana Hovig at the Bill and Melinda Gates Foundation) shows a five year lag in the US for vaccines and drugs. As one of 26 Community Educator Scholarship Awardees at this year’s Conference on Retroviruses and Opportunistic Infections (CROI), it is my goal to help reduce that delay by focusing on research that has the potential to impact community members and frontline workers who I interact with on a daily basis in the short term.
I am sure that scientists and advocates will spend the next year talking to each other about the issues and information that came from oral abstract sessions reporting on long-acting cabotegravir (Abstract 83) and dapivirine ring studies (Abstract 143LB and Abstract 144LB). Advocates should also be engaging community members and frontline workers in conversations about these emerging tools for HIV prevention.
Almost six years after FDA approval, oral PrEP is a part of the HIV prevention landscape worldwide, but it looks different depending who you are and where you live. PrEP access still seems to be among the most relevant issues for HIV-negative black MSM in the United States, while viral suppression (which is key to improving health outcomes and eliminating the risk of onward transmission) remains a priority concern for PLHIV. Do PrEP and treatment as prevention really give us all of the tools we need to end the HIV epidemic? What follows are a few of my (US-centered, black MSM-focused) highlights from #CROI2018:
Oral Pre-Exposure Prophylaxis (PrEP)
Does PrEP drive STI rates? No! Abstract 1025 looked at condom use patterns in about 300 MSM and transgender participants in a PrEP pilot study. Reported condom use did drop, but overall rates of STI diagnosis didn’t not rise. The investigators conclude that “neither overall condom use nor change in condom use were associated with STI diagnosis.” Good predictors of STI diagnosis among PrEP users included being under 25 years old, being diagnosed with an STI in the 6 months prior to starting PrEP, and the number of sex partners. The researchers conclude that “particular attention and support is needed for younger PrEP users,” and, “although many PrEP prevention messages stress condom use, the number of partners appears to be a more important predictor of STI diagnosis among PrEP users.”
…and, in an exploration of the intersection of PrEP and STIs in the United States, Dr. Julia Schillinger said, “as researchers are looking at retention on PrEP, maybe one of the things they could also measure is, even if people aren’t retained on PrEP, are they retained in a system of testing and primary care?”
Should PrEP be prescribed for people who use meth? Yes! Starting with data from the iPrEX study and its open-label extension, it’s been clear that people at risk of HIV and unable to use condoms will use PrEP correctly and consistently. A study of these issues at CROI found more evidence of this. The study enrolled MSM who were using PrEP and reported condomless anal sex with multiple partners (CAS-MP). Some also reported stimulant use. The researchers wanted to know how stimulant use and condomless anal sex affected adherence to PrEP. They measured the presence of PrEP in blood samples from the study participants. (This can give a more accurate picture of whether people are taking PrEP than their own reports. Overall, 80 percent of participants in the study had protective levels of PrEP in their blood over the course of the 48 week study, regardless of stimulant use or frequency of condomles anal sex.) Conclusion: “Stimulant use should not be a deterrent to prescribe PrEP to high-risk individuals engaging in CAS-MP.”
Short-term PrEP as part of vacation package??? Yes! Advocates have stressed for years that oral PrEP is not forever. Rather, it should be used during a person’s “season of risk.” Sometimes those seasons aren’t very clear. Sometimes they are. Researchers investigating the feasibility of short-term, fixed interval, episodic PrEP (epi-PrEP) found in a study of 54 men who have sex with men (MSM) that most were adherent during short, high risk vacation periods. Study participants started oral PrEP 7 days prior to vacation and were instructed to adhere to daily dosing through seven days post-vacation. (They also received a single session of cognitive behavioral therapy at least two weeks before the vacation.) Nearly 94 percent of the men in the trial had protective levels of tenofovir-based PrEP in their blood at a study visit three days after their vacation was over. Epi-PrEP may be a good option for some men with episodic high risk for HIV infection, and as an added bonus, “initiating PrEP on vacation may provide a helpful way to initiate long term PrEP.”
Oral tenofovir-based PrEP is still one of the most important tools for HIV prevention available today, but it is not a magic pill. Dr. Roel Coutinho reminded CROI attendees that using PrEP to eliminate HIV would take about 80 to 120 years without including other HIV prevention strategies. This is why viral suppression for people living with HIV is still a priority.
Viral Suppression
Findings from CROI:
- Higher HIV viral load was independently associated with the likelihood of transactional sex. Additionally, those testing positive for an STI were nearly twice as likely to report transactional sex as compared to those without STIs.
- Decreasing alcohol use without abstinence from alcohol was associated with a lower viral load. In other words, people with HIV whose drinking interferes with adherence to medication may be better able to take their medications when they reduce their drinking-without completely stopping. This can inform counseling messages and harm reduction approaches.
- A study of PLHIV living in the San Francisco Bay Area got nuanced about types of homelessness-which can range from living outdoors to crashing with friends or family. It looked at the relationship between different types of homelessness and virologic suppression. Although living outdoors was associated with the lowest proportion of viral suppression, other forms of unstable housing (including living in a shelter, ‘couch-surfing’, and being in an single-room occupancy) were also associated with lower levels of viral suppression compared to renting or owning. Interventions are needed to increase viral suppression among PLHIV across a spectrum of unstable housing arrangements.
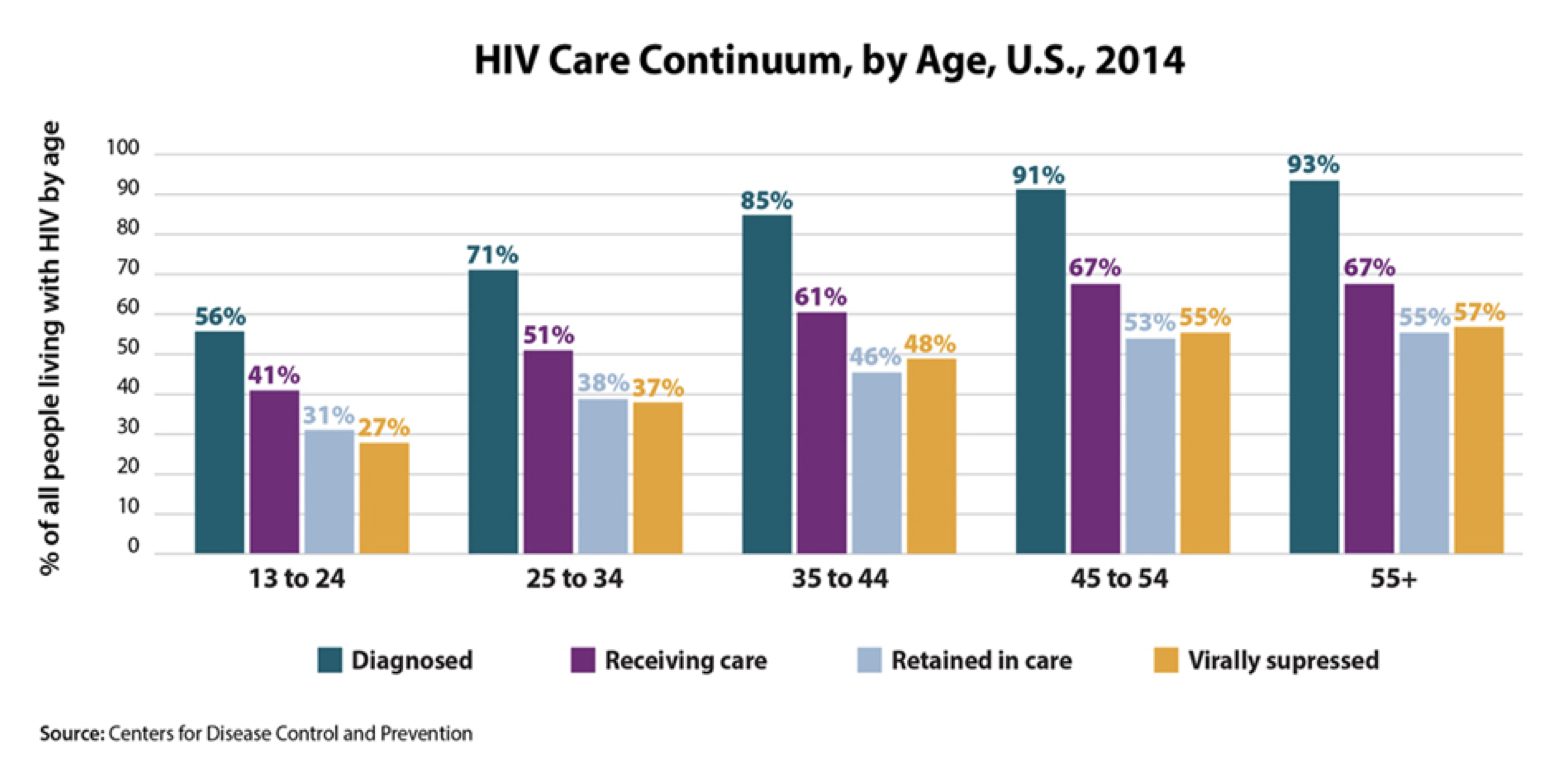
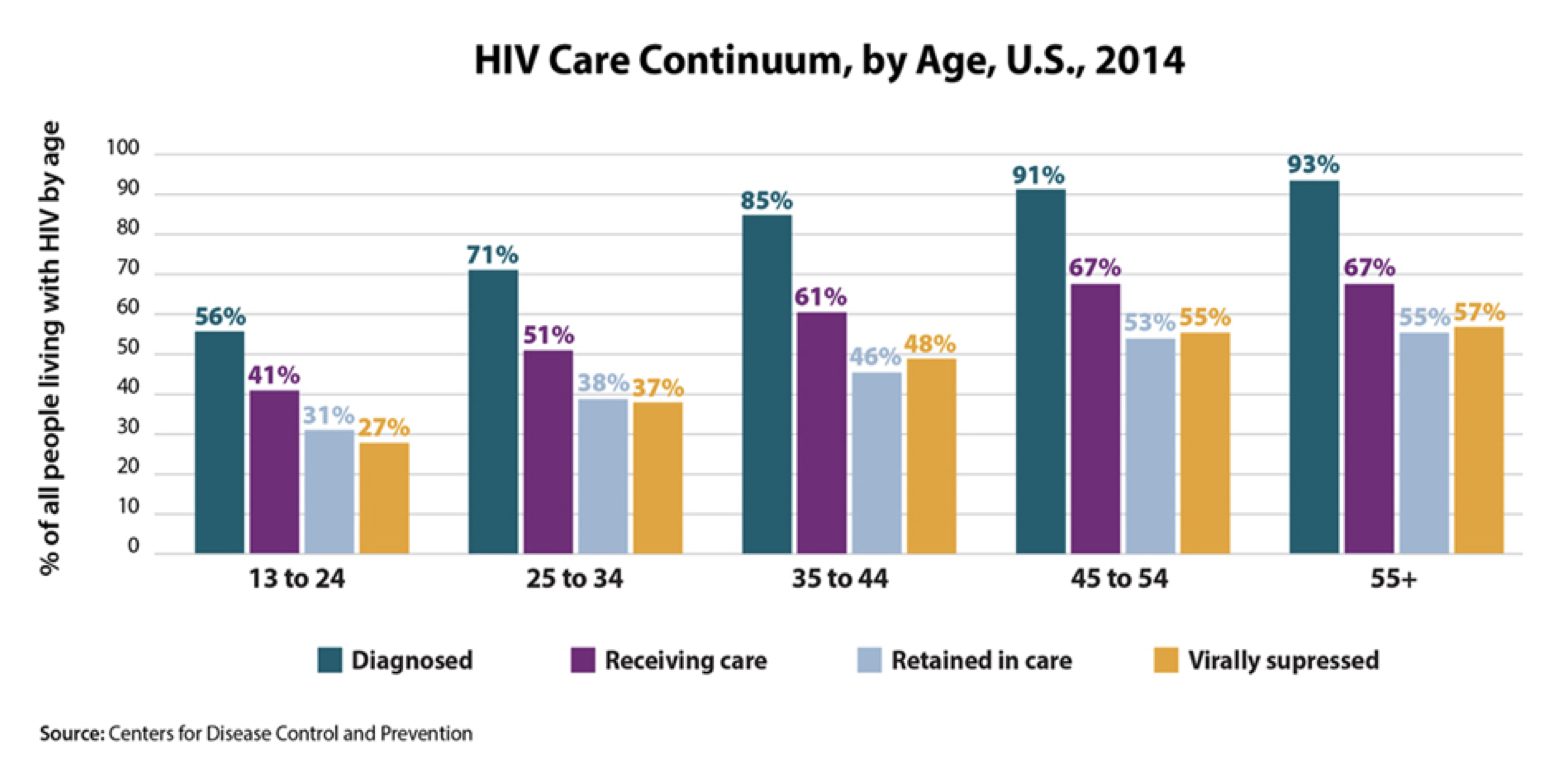
- More frequent social work visits and nurse phone calls were associated with retention in care for young adults with HIV, but improved retention did not to lead to improved viral suppression. In general, young adults have lower rates of antiretroviral use and medication adherence than older adults, so lower rates of viral suppression in this group should come as no surprise. CDC’s HIV Care Continuum by Age shows that young people living with HIV are less likely than older Americans to be diagnosed, to be in care, and to be virally suppressed. Socioeconomic challenges, depression, and lack of tailored interventions to improve adherence among young people are among the issues that must be addressed to improve viral suppression for young adults with HIV.
So much information, so little time. This year’s CROI featured lots of research focused on women, hepatitis C, tuberculosis, anal cancer, and a host of other issues that will continue to be analyzed and reported over the next several months. My initial brain dump to frontline staff at APEB was intended to share information that they might find useful in their work with members of our community now. We’ll continue to develop workshops and presentations and events that attempt to keep folks armed with the latest information available and prepared for what’s coming next. Somewhere between “now” and “next,” we have a lot of work to do!