October 10, 2024
Access, access, access. At the plenary Back to the future, Sharonann Lynch of Georgetown University called for a transformational approach that would harness ambition and finally disrupt the “mediocre pace of scale-up” that squandered the global opportunity to leverage oral PrEP in 2012 and bend the curve of the epidemic. Instead, the world saw the slow and fragmented 10-year rollout of oral PrEP. In this alternative vision, donors and global health leaders can and must create the conditions for both high demand of promising HIV prevention options and, ultimately, affordable choices by investing now in large volumes of new interventions such as injectable lenacapavir (LEN). Without this ambition, cautious investment will signal low expectations for demand, resulting in “a massive chilling effect” on the timelines for generics and delays in access to more affordable products. “It will ration eligibility and result in the slow drip of uptake,” said Lynch.
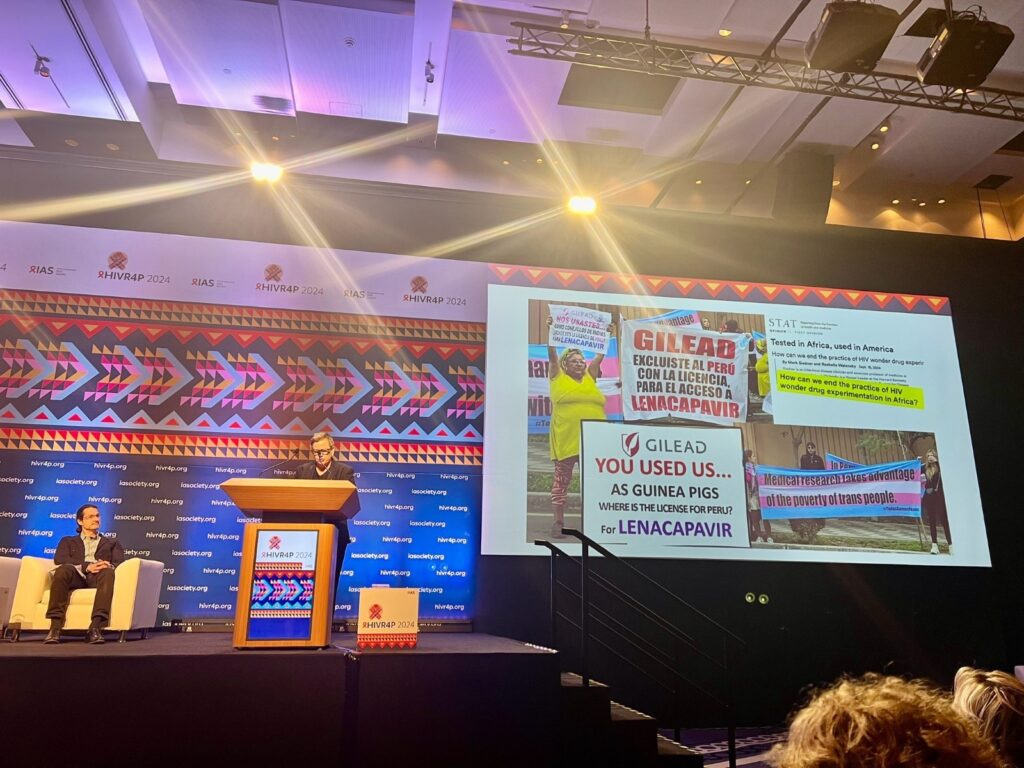
Lynch also called for access to generic injectable lenacapavir (LEN) to places where the HIV epidemic is concentrated, regardless of the wealth status of the country. Gilead Science’s licensing agreement with six generic manufacturers does not include the middle-income countries that hosted the PURPOSE 2 trial testing LEN for PrEP, including Peru (the conference host country), Brazil, Argentina, Mexico. This was one of the talking points of a protest from the trans advocacy group Féminas Perú who highlighted that vulnerable communities are often used for research and the outcomes fail to benefit targeted populations. “We are more than just studies” they said at the demonstration on Monday.
See AVAC’s updated Lens on LEN, and new Plan for Accelerating Access to Injectable Lenacapavir for PrEP for details on what must come next for LEN to successfully act on Sharonann’s and activists’ calls to action.
At the conclusion of the plenary, Gastón Devisich of Fundación Huésped was honored as the recipient of the 2024 Omololu Falobi Award for Excellence in HIV Prevention Research Community Advocacy. Presented biannually in honor of Omololu Falobi who helped transform advocates’ roles in HIV prevention research, Devisich embodies his legacy, helping to raise the profile of critical research in Latin America and ensuring the inclusion of the LGBTQ+ people in clinical trials. “Access is a fundamental human right,” Gastón said in his acceptance speech. Read more about Gastón Devisich and the Omololu Falobi Award in our press release.

A longer-acting PrEP ring and a nonhormonal MPT?
New data on a three-month dapivirine vaginal ring (DVR) was presented at a session on late-breakers. An open label, Phase 1 study compared pharmacokinetics (PK) of a three-month DVR with the approved one-month DVR. The rings are identical except the longer-acting DVR contains 100 mgs of dapivirine, compared to 25 mgs in the monthly ring. Data showed no difference in safety and demonstrated the PK superiority of the 3-month ring, “suggesting efficacy of the three-month ring will be at least equal to the one-month ring,” said Jeremy Nuttall of the Population Council who presented the findings. The Population Council ultimately intends to pursue regulatory approval and expects a longer-acting DVR, requiring 4 rings per year instead of 12, to reduce production cost by as much as 60% and ease the burden on both ring users and health services.
Sanyukta Mathur, also of the Population Council shared findings from a national online survey of women in the US regarding their preferences for a nonhormonal ring in the session, Prevention advances: PrEP, DoxyPEP and MPTs. Using a hypothetical target profile of an MPT vaginal ring—it lasts for a month; offers 80% effectiveness at preventing pregnancy and 50% effectiveness in preventing HIV and STIs; contains no hormones and has no impact on their menstrual cycle—researchers found that nearly 3/4 of all women would likely or very likely want to use this ring. The highest interest in this product was from older women who already had children, and those who perceived themselves to be at high risk for HIV acquisition.
STI prevention: We need to do more!
Diagnostics are key to making progress against STIs around world, according to presentations at the session STI prevention: We need to do more. Judith Kyokushaba from the Ministry of Health, Uganda presented findings that multipurpose rapid tests were highly acceptable, usable, and feasible by health workers to detect HIV, syphilis and hepatitis B in Uganda among pregnant women attending antenatal care health facilities. Scaling up these tests and making them accessible throughout Uganda and worldwide is the challenge for the field.
Thesla Palanee of Wits RHI drew parallels between the STI and HIV epidemics at the session. Africa is faced with a growing STI epidemic, with many asymptomatic infections, which leads to a lack of awareness and continued transmission. Because of cost, many countries rely on patient reporting of symptoms (syndromic management), which is ineffective. The lack of available diagnostic tools hinders effective prevention and management of HIV and STIs. More accessible point-of-care tests, as well as better screening tools to identify asymptomatic infections are imperative. As one session participant said, “We need to get a community advocating for continued diagnostic and testing.” We couldn’t agree more. See AVAC’s STIWatch.org website, a new resource to support communities to better understand and advocate for STI vaccine and diagnostics research, development and rollout.
Increasing bNAb options: Target product profiles for prevention strategies
Nyaradzo Mgodi opened the session, Increasing bNAb options: Target product profiles for prevention strategies by asking, “in this era of antiretroviral excitement, are bNAbs still relevant?” The answer is YES, she said. “bNAbs are on the path to join the prevention toolbox, alongside condoms, pills, injectables, and structural/behavioral interventions.” Despite this robust prevention toolbox, the world still has unacceptably high HIV incidence. Presenters discussed progress in bNAb research, but disappointingly, the session did not include mention of a target product profile (TPP), which, as we’ve heard from the People’s Research Agenda, is critical, as the field envisions a prevention pipeline that serves communities.

Misinformation, fear-based approaches and other challenges hindering progress
A session focused on breaking a paradigm of stalled progress in rolling out effective prevention, Reducing burdens and barriers to expand the use of HIV prevention options, featured research and initiatives with vital lessons for the field. Yvette Raphael of the African Women Prevention Community Accountability Board (AWPCAB) said “Biomedical prevention is at a turning point, but success depends on countries and funders to heed evidence-based demands of advocates and emphasize choice over products, both long-acting and user controlled.” See the AWPCAB’s Choice Manifesto to learn more.
Michael Stirrat of the US National Institute of Mental Health described strategies to overcome misinformation and its pernicious effects on public health, that include vaccine skepticism, reduced PrEP adherence, and adverse health outcomes among marginalized communities. In addition to a list of “do’s”, such as tailored messaging by community, leadership from trusted messengers and framing public health interventions as a social norm, Stirrat called for investment in communication research. And he presented results from examples that used “pre-bunking” to make advanced communication investments in communities with accurate information.
Sarit Golub from Hunter College of City University of New York presented on the urgent need for the research community to examine and transform an ineffective fear-based and risk-oriented approach to public health, from screening tools to research questions. Calling this approach “the most harmful” impact of the field, Golub called for assessments, counseling strategies and research tools across the board to commit to approaches that put less focus on which methods of HIV preventions people adopt and more focus on sexual well-being and how to make their choices work for them.
“Nobody identifies as “high-risk” and nobody goes out on a Saturday to have “risky behavior,” said Golub.

Lessons in implementing PrEP, DoxyPEP and MPTs locally & in key populations
Implementing PrEP, DoxyPEP, and MPTs in local communities and among key populations is where the rubber meets the road. Wednesday’s session Prevention advances: PrEP, DoxyPEP and MPTs highlighted studies on delivering these options to communities. One presentation featured Project PEACH, a study on PrEP and DoxyPEP use among MSM in Atlanta, GA. Of 240 participants (63% Black, 17% Latino), 219 chose PrEP (166 daily oral, 43 on-demand, 10 LA-CAB). Among PrEP users, 74% also opted for DoxyPEP, 18% chose only PrEP. 7% of the study participants chose doxyPEP only, and 2% stayed engaged via the study app without using either.
Of the 100 participants who completed follow-up, 20 chose to switch their initial form of PrEP, with most moving from daily oral PrEP to either 2-1-1 dosing or LA-CAB. This is significant, as past research shows young Black MSM often stop PrEP after a few months. According to study presenter Oumaima Kaabi, “offering comprehensive and flexible sexual health options, along with motivational interviewing, can enhance persistence.”
A study in Milan, Italy, involving 754 MSM, assessed the impact of DoxyPEP on bacterial STI rates over two years. Angelo Roberto Raccagni presented findings showing that 222 men reported using DoxyPEPafter being prescribed it. Among users, there was an 87% reduction in chlamydia, 80% in syphilis, and 74% in gonorrhea (the latter consistent with other studies showing DoxyPEP’s lower effectiveness against gonorrhea), in a region with higher rates of drug-resistant gonorrhea among MSM. See AVAC’s guide to DoxyPEP for more.
There is much more to come in Lima, so be sure to look out for our ongoing coverage and see reports from earlier this week here and here.