A detailed graphic describing the status of pre-clinical and clinical work around relevant bNAbs today.
HIV-Specific Neutralizing Antibodies: A guide to targets and candidates
Where Does Oral PrEP Fit in to Vaccine and AMP Trials?
A global map showing current efficacy trial countries and their status of PrEP implementation.
Vaccines and Antibodies on Efficacy Pathways
A timeline of current efficacy programs for vaccines and antibodies, highlighting the P5 program testing pox-protein candidates, the Janssen program testing mosaic-based candidates, and the AMP studies testing the antibody VRC01.
New Px Wire: Trial design in the era of PrEP
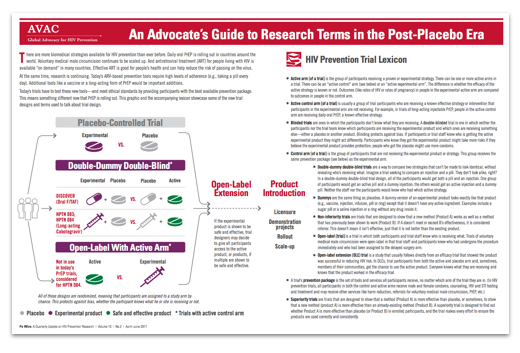
Our new issue of Px Wire offers an advocate’s guide to some new types of biomedical prevention trial designs.
Next-generation PrEP products include long-acting injectable ARVs (which are also being tested for treatment in people living with HIV). How do you find out if injectable PrEP is better, or as least as good as, daily oral PrEP? The new trial designs hold possible answers.
In this info-rich Px Wire, you’ll find a handy summary of long-acting PrEP trials, a lexicon of key terms for the “post-placebo era”, and a handy illustration for looking smart while you explain “double-dummy double-blind”.
An Advocate’s Guide to Research Terms in the Post-Placebo Era
In Px Wire, AVAC’s quarterly update on HIV prevention design, we presented this illustration on some new types of biomedical prevention trial design. You’ll find a summary of long-acting PrEP trials, a lexicon of key terms for the “post-placebo era”, and a handy illustration for looking smart while you explain “double-dummy double-blind”.
To download just the graphic, without the accompanying text and lexicon, click here: JPG, PDF. For the lexicon only, click here (PDF).
AIDS Vaccine Science for Busy Advocates: Antibody Research
A primer on antibodies and their role in HIV prevention research. Read on for a glossary of relevant terms and to learn how broadly neutralizing antibodies may be important to the development of a vaccine.
AVAC’s Month-Long Vaccine Immersion Continues: Webinar series, cheat sheets and more!
[UPDATE:] Recordings of webinars already held are now available below.
Join us in our month-long “deep dive” into the dynamic field of HIV vaccine research with the next installment in our HIV Vaccine Awareness Day webinar series coming up this Thursday—a review of the NIH’s Vaccine Research Center with Barney Graham. And read on for links to key resources, including quick references and a recording of our first webinar.
Webinar series lineup:
- Friday, April 28: Ad26 Mosaic Program—Janssen’s Maria Pau discusses preparations for the next efficacy trial.
YouTube / Audio / Slides - Thursday, May 4: The History—and Future—of the NIH’s Vaccine Research Center with Barney Graham.
YouTube / Audio / Slides - Monday, May 8: Building on (and Building!) Success—Status of HVTN 702 with Fatima Laher.
YouTube / Audio / Slides - Thursday, May 11: “Plan B”-NAb? An Overview of Antibody Research with Lynn Morris.
YouTube / Audio / Slides - Thursday, May 18: An Overview of Vaccine Development from Julie Ake of MHRP.
YouTube / Audio / Slides
Last Friday, the series launched with an overview from Janssen’s Maria Pau on the Ad26/Mosaic vaccine program—notable both for its science and for active leadership from industry. Two of the upcoming webinars will fill advocates in on bNAb research. Broadly neutralizing antibodies—bNAbs—are anti-HIV proteins now being tested for efficacy as HIV prevention through direct “passive” infusions. The upcoming discussions will help answer burning questions for HVAD 2017:
- Which bNAb candidates should we be watching in the coming years?
- What do bNAbs mean for HIV vaccine research? Are these current trials, testing direct infusion of bNAbs, a pathway to a new product or a way to advance the HIV vaccine field—or both?
- What will current large-scale efficacy trials of vaccines and bNAbs tell us?
We know not everyone hears bNAb and immediately understands the term. This year, AVAC has updated our series, Vaccine Science for Busy Advocates, to provide quick, clear explanations, with a focus on topics corresponding to our webinars. Click here to access Busy Advocates: bNAbs. Download it, review the terms and be ready with your questions on May 4 and May 11.
There’s a lot to know. But the research is promising, and we need steady hands on deck to ask smart questions and sustain support. Continue with us over the next several weeks on the countdown to HVAD to play your part.
CROI 2017: A View from My Seat at the Table
The annual Conference on Retroviruses and Opportunistic Infections (CROI) is an annual gathering where advocates and researchers learn where the science on HIV is taking us. The findings can be both grand and granular. They answer questions, raise new ones or both. And not all of those questions are strictly about science. Two of AVAC’s partners have been reflecting on what they took away from the conference, insights that inform our thinking long after the sessions end and results are published.
Rob Newells is an Associate Minister at the Imani Community Church in Oakland, California, and serves as Executive Director for AIDS Project of the East Bay—a community-based organization serving the most vulnerable and marginalized communities in Alameda County since 1983. He was a 2011 Fellow of the Black AIDS Institute’s African American HIV University Community Mobilization College and has been a biomedical HIV prevention research advocate with AVAC’s US PxROAR group since 2012.
There are conferences that I attend where I can be “Rob Newells, Executive Director for AIDS Project of the East Bay (APEB).” The Conference on Retroviruses and Opportunistic Infections, more commonly known as CROI, is not one of those conferences. At CROI, the ED hat comes off, and I’m purely a community advocate again. This year, that was even more true than in previous years. As I looked around the room of Community Educator Scholars (a program that supports advocates attending CROI) as we gathered for our first early morning breakfast of the week, I immediately noticed that I was the only African American man at the table. There were two African American women (one Scholar and one member of the Community Liaison Subcommittee) and several Africans (shout out to my brothers Ntando, Simon and Supercharger), but no other Black men from the United States. It wasn’t the first time that I’ve been the only one, and I know it won’t be the last, but—if I’m being honest—I was both disappointed and stressed by it. I felt a lot of pressure to be the eyes and ears for my community in a way that I hadn’t felt in previous years.
From a community perspective, CROI is the most boring meeting I attend. It’s 4,000 science and research geeks talking to each other about what they’ve been doing locked away in their labs for the last few years. Most of the news that gets reported after CROI is for science and research geeks, and those reports usually miss the things that I find interesting or that I think my community would find interesting, useful, and relevant. So, in an attempt to rectify that shortcoming, I attended all of the plenary sessions and a bunch of the oral abstract sessions and even took my time to talk to presenters during the poster sessions. I took lots of notes and pictures of slides, and when I returned home (after another conference the following week) I talked it all through with my staff. It took a while longer for me to organize my thoughts into a coherent presentation that I could use for the community report-back I coordinated at the Alameda County Public Health Department on National Women and Girls’ HIV/AIDS Awareness Day. This is some of what I shared.
CDC’s oral presentation on HIV Incidence, Prevalence and Undiagnosed Infection in Men Who Have Sex with Men gave us good news and bad news. The good news is that the percentage of undiagnosed HIV infections decreased for all racial/ethnic groups between 2008 and 2014. (That tells me we’ve been doing a better job of testing.) The bad news is that there was an increase in HIV incidence among Latino MSM and MSM between the ages of 25 and 34. (Annual infections among Black MSM dropped from 10,100 in 2008 to 10,000 in 2014. I don’t see that as anything to write home about, but a decrease is a decrease, right?)
Anal Cancer
I had my third or fourth high resolution anoscopy (HRA) just before CROI, so I was particularly interested in a few of the abstracts related to anal cancer. (There were seven posters and four oral abstract presentations on anal cancer this year, so I wasn’t the only one interested.) While anal cancer is fairly rare overall, men living with HIV who have sex with men are 60-190 times more likely to get anal cancer than the general population. We know that certain types of HPV are responsible for most anal cancers, and most MSM living with HIV have HPV of one type or another. What we didn’t know was what we should be doing about it. What I took away from CROI 2017 was that anal cancer screening should start at 30 to 35 years old for MSM living with HIV. Insured folks like me should get an annual HRA. Unfortunately, HRA is not the most cost-effective prevention tool, and resources to perform the test are limited worldwide. Additionally, patients who rely on the Ryan White AIDS Program or Medicare for coverage have to settle for a digital rectal exam (exams where the doctor inserts a gloved, lubricated finger into the anus to feel for unusual lumps or growths) to detect anal cancer because an HRA isn’t covered. As fun as a digital rectal exam may sound, it’s not that effective. HRA detects the most cancers. (I know from personal experience. I asked my primary care physician to refer me for an anal pap smear and HRA a few years ago. He didn’t find anything suspicious with the digital rectal exam, but he gave me the referral anyway. The HRA found a stage 4 pre-cancerous lesion which was removed during the procedure. Thank you, Kaiser Permanente.)
Antibodies
Bridge HIV in San Francisco is one of the sites for the AMP (antibody mediated prevention) Study, and I know people in my community who are enrolled so I paid attention. Antibodies are a big deal in HIV research. My takeaway from CROI was that the current study won’t produce a home run that will work for everyone. Researchers hope to have an understanding about whether or not antibodies can work for prevention, but as public health intervention it is cumbersome, involving monthly clinic visits and transfusions. And no matter the results from AMP, vaccines based on neutralizing antibodies are still a long way off.
Cure Research
There were two things I found interesting in the cure research presented this year. The first was that people on effective antiretroviral therapy are not producing new HIV-infected cells. Cells proliferate before they die off. That means that earlier detection and treatment results in fewer proliferating cells with less diversity and smaller reservoirs. That might make HIV easier to target and cure. The other thing that caught my attention was that estrogen blocks RNA replication. That discovery leads to at least two pathways to cure: Can we block estrogen to bring latent cells out of hiding (the “flush and kill” strategy), or can we increase estrogen to keep RNA blocked (the anti-proliferation model)?
Drug Use and MSM
Over the past few years, I have heard from friends in Oakland and Atlanta that there was an increasing problem with crystal meth use among Black MSM. I’ve had conversations with many of my colleagues about the increasing mention of PnP (Party and Play) on dating/hook-up app profiles. For years, the common assumption has been that meth is for white boys, but apparently more and more black men are going that route. There were a couple of posters about drug use and MSM that I totally expected to confirm that for me. The first, from CDC, looked at drug use by MSM in 20 cities across the United States. Surprisingly, they didn’t see an increase in meth use. They saw an increase in prescription opioid use among Black MSM between 2008 and 2014. But just two steps away, the very next poster from George Washington University noted a drastic increase in crystal meth use among Black MSM in Washington, DC, over the same time period. I totally expect to see more research in this area.
Pre-Exposure Prophylaxis (PrEP)
What I heard coming from Seattle about pharmacist-managed PrEP was intriguing. Being able to avoid the cost of a clinic visit could greatly increase access and uptake. I contacted my agency’s pharmacy partner when I got home to find out if they had the ability to order labs and prescribe Truvada for PrEP without patients having a clinic visit. (They can, and we will.)
And there was good news for women. Apparently, there was some confusion after all of the talk about good and bad bacteria in the vaginal microbiome at AIDS 2016. That was in relation to vaginal microbicides. Oral PrEP doesn’t go through the vagina, so the vaginal microbiome has no effect on blood and tissue levels of the drug. Oral PrEP works for women. Period.
There were a few other abstracts dealing with community cohort care for adolescents, HIV testing incentives, and text messaging interventions for PrEP users that were interesting enough for me to mention to the folks at home, but if I’m being honest, I was looking for something else.
CROI 2017 was the first conference in an entire year where I didn’t hear anything from the HPTN-073 team. Instead we heard from a team at Emory University, but what I heard only annoyed me. I don’t need another study that tells me how Black MSM don’t use PrEP. The study led by black men for black men (HPTN-073) showed us what works. Emory presented yet another study that showed us what doesn’t work. They studied Black MSM aged 16 to 29 in Atlanta. Participants were offered risk reduction counseling, condoms and lube, and non-incentivized oral PrEP. After viewing a brief education video from WhatIsPrEP.org, the men who expressed interest were scheduled to see a study clinician to initiate PrEP.
The study results indicated that 56 percent of the men expressed interest but 39 percent of those never showed up for the initiation visit with the clinician. Of the ones that did come back, only 35 percent initiated PrEP. The study team’s conclusion was that, “even after amelioration of structural barriers that can limit PrEP use,” PrEP uptake was suboptimal. What structural barriers, you ask? Only lack of health insurance was addressed. (As if that’s the most pressing structural barrier Black MSM face in the United States.) When I asked about what else was done to engage these men based on what we know from HPTN-073, I was told that there is really “no hard, a priori evidence that more aggressive interventions are needed” for Black MSM.
I sat down so that I wouldn’t come off as the angry Black man, but when 79 percent of the participants in HPTN-073 accepted PrEP after a series of counseling sessions that combined service referral, linkage and follow-up strategies to address unmet psychosocial needs (part of what that team calls C4, or client-centered care coordination), I would argue that the need for more aggressive interventions is obvious. A study led by black men told us how to work with black men. Apparently, someone needs to fund more “For Us, By Us” studies so that we have a body of evidence showing what works because I’m tired of hearing what doesn’t work.
There were no exciting results from large efficacy trials at this year’s CROI like there have been for the last several years. It was back to basic science. That means the conference was even more boring than it normally is. But when I returned to Oakland and put my E.D. hat back on, I realized that I had the power to implement some of what I learned without waiting for studies to be published or government agencies to catch up to the science which could take years. I had the power.
In addition to client-centered care coordination and pharmacist-managed PrEP, we are in the process of adding an optional SMS intervention to the PrEP program at APEB, and we’ve started working with La Clinica de la Raza—a local community-based organization that prioritizes Latino populations—to support efforts to address the increasing HIV infection among Latino MSM. That’s why I go to CROI. That’s why I’m grateful to the scholarship committee for supporting my attendance and to AVAC for always providing what I need in order to stay on top of new developments in biomedical HIV prevention research. That’s why I wish I wasn’t the only African American man at those daily 7am breakfast meetings.
…cue Solange’s “F.U.B.U.”
Dear HIV Researchers, To Do Effective Research – Engage Us
The annual Conference on Retroviruses and Opportunistic Infections (CROI) is an annual gathering where advocates and researchers learn where the science on HIV is taking us. The findings can be both grand and granular. They answer questions, raise new ones or both. And not all of those questions are strictly about science. Two of AVAC’s partners have been reflecting on what they took away from the conference, insights that inform our thinking long after the sessions end and results are published.
Julie Patterson is an HIV prevention research advocate and public health professional who lives in Northeast Ohio. She is chair of the Case Western Reserve University/University Hospitals of Cleveland AIDS Clinical Trials Unit’s Community Advisory Board, a member of AVAC’s PxROAR program, and a member of the US Women and PrEP Working Group.
Recently, I had the opportunity to attend the Conference on Retroviruses and Opportunistic Infections (CROI) as a community educator scholar. It was a grand experience – a gathering of brilliant, hard-working research minds at one of the premier HIV scientific meetings that are held each year. It was truly an honor to be among them.
However, I’m not sure my presence was felt.
A cohort of us came to CROI to give voice to community needs and bring new research back to our communities. We see it as a two-way street.
On the first day of CROI, there is a workshop held for newer researchers called, “Program Committee Workshop for New Investigators and Trainees”. People awarded the Young Investigator and International Delegate Scholarship are required to attend in order to get an introductory overview of the conference, what to expect in the days ahead, and a primer on aspects of the science that may be unfamiliar. The attention is on the science and the scientists—new investigators and clinicians who are actively involved in research. The organizers encourage participants to ask questions because lab scientists aren’t always aware of the issues in epidemiologic research, virologists speak a slightly different tongue than immunologists. You get the idea.
Not surprisingly, community educators are also required to attend the workshop for new investigators. This is a great idea; the nature of these talks is more general than others at the conference, and provides a foundation for understanding key results. Unfortunately, the structure often does not allow the presence of community educators to be known. Sure, we ask questions, but mostly we are like ghosts – ethereal beings with messages from the past. Not quite real. Certainly not equals.
This year, in what I perceived as an attempt to turn this CROI norm on its head, one of the crucial lectures included in the workshop was centered on GPP—Good Participatory Practice. It was led by community activists, grounded in the lives of people living with HIV, and aimed squarely at the new investigators, and with this I agree wholeheartedly. The Martin Delaney Lecture honored his legacy and brought the attention back around to the communities who are struggling with HIV, to the people who are at the heart of this epidemic. The message: listen to community stakeholders, and you will hear what you need to know. Ignore them, and your research results will suffer. We will all suffer.
I was disappointed that this vital talk was held during lunch when many left the room to pursue other food options. Most of the awardees of the Young Investigator and International Delegate Scholarship stayed to eat a free box lunch, but the timing appeared to indicate that this lecture wasn’t as important as the others. It would have been easy to miss it and not be held accountable.
Researchers, I’m here to say that you are accountable to us. We need you on our side and to see this through to the end. Our goals are the same—we want to end this HIV epidemic, to roll out a vaccine that will prevent new infections, to find a cure that works for everyone, to lead happy, healthy and long lives full of purpose and meaning, full of love and adventure. We want to see all of it in our lifetimes, just like you.
I tend to follow HIV prevention and public health research closely, so those were the sessions that I attended. Time and again, I sensed the urgency in the tone of the presentations. For that I am grateful. We must continue to push forward. Yet I also heard something else, even from prominent scientists—a scientific expediency that can leave communities behind.
Two significant HIV prevention clinical trials that are currently being conducted under the umbrella name of the “AMP Studies”—HVTN 704/HPTN 085 and HVTN 703/HPTN 081 are a case in point. I sit on the Community Working Group for these trials that are studying the efficacy of antibody mediated prevention. The HVTN 704/HPTN 085 trial is recruiting cisgender heterosexual women at risk in South Africa. In the US, Peru, Brazil and Switzerland, HVTN 703/HPTN 081 is recruiting cisgender men and transgender people who have sex with men.
Unfortunately, on multiple occasions at CROI, when I heard researchers refer to the AMP Trial, they neglected to mention the involvement of transgender people.
This may seem like a small oversight. Surely it is acceptable to use shorthand amongst fellow researchers? Everyone knows that referring to MSM as the target population for recruitment in this situation includes transgender people, right? Wrong. Transgender and gender non-conforming (TGNC) people don’t necessarily assume it. We all need to see ourselves in HIV prevention research.
Will this study collect data in such a way that we can separately analyze findings that are specific to TGNC participants—if not,we will have lost an invaluable opportunity. Will TGNC people at risk for HIV see results from AMP as applicable to their lives? If our experience with PrEP is any indicator, the answer is no, unless the investment continues to be made in TGNC people. AMP has included TGNC stakeholders early in the research process- from choosing research questions to protocol development, from design of informed consent to rollout of marketing materials. Now advocates are watching to ensure that it continues—from interpreting results to follow-on studies and implementation, all the way to the next trial. Every step of the way. Every step.
The AMP Trial has helped to set a new standard for transgender inclusion in HIV prevention research, but it is only one example of how GPP can be utilized. There are so many more. Community stakeholders have to be involved at every step.
In the end, researchers, my message isn’t to watch your step, it’s to walk alongside us. We can’t do it without you, and you can’t do it without us. As community stakeholders, we bring information to the table that you may never know without our voices. Knowing it up front will make the science more efficient, more ethical, and better in the long run.
For over 30 years, HIV research has been on the cutting edge of engaging affected communities and working together with activists. We need to keep that momentum going. I look forward to it.
Editor’s Note: AVAC’s Stacey Hannah led the presentation during the session on Good Participatory Practice (GPP). GPP is a set of guidelines developed by AVAC and UNAIDS in 2007 to engage affected communities and all other stakeholders in the design and conduct of biomedical HIV prevention trials. GPP has been widely adopted and is instrumental to a research process that yields trusted results.
What’s New on AVAC.org
AVAC.org has a host of new resources providing concise updates, informed perspective and handy tools. Take a look at the highlights below and get up to speed on a range of strategic issues.
New Resources
- AVAC, in partnership with the Clinton Health Access Initiative (CHAI), is taking on new work focused on supporting innovation in the prevention “market”—including the programs that deliver new products and the pipeline of products in trials. This two-page intro to the “HIV Prevention Market Manager” gives an overview of this new body of work.
- To get a flavor of the work the Prevention Market Manager team is focused on, check out this new resource: End-User Research Landscape Mapping and Findings. The term “end user” is used by people who work on developing and marketing products. It refers to the individual who’s ultimately going to make the decision to seek out and use a given product or intervention. This resource gives a sense of the range of efforts trying to understand what is and isn’t known about one key set of “end users” for new prevention options—adolescent girls and young women in sub-Saharan Africa.
From the Infographics Gallery
- The Years Ahead in Biomedical HIV Prevention Research provides an overview of the current and planned efficacy trials for the major biomedical interventions under investigation right now. The infographic is the centerspread in the current issue of Px Wire, which looks ahead to a host of issues we are watching in 2017.
- Introduction to Long-Acting Injectables is an updated graphic to guide you through the basics of antiretrovirals that are being developed as long-acting injectables for both treatment and prevention.
Strong Voices in P-Values
- Progress and justice for women and girls has come under attack by the new US administration via the reinstatement and proposed expansion of the Global Gag Rule. In Standing Together Against the Global Gag Rule the AVAC team reaffirms its commitment to the fight for bodily autonomy, for justice, for choice and voice for women and girls.
- In New and Touted HIV bNAb: Big deal or news blip?, veteran science writer and HIV journalist Mark Mascolini delves into the nuances of vaccine research using broadly neutralizing antibodies. You will learn more than just what these are; Mascolini looks at the big promises and the small print.
- Lindsay Roth, a long-time organizer and advocate for sex workers’ rights, gives any lay reader on the subject of sex work an opportunity to gain a deeper understanding of the issues at stake in Getting Set to Defend and Advance Sex Workers’ Rights in 2017 and Beyond. Roth’s reporting shows how HIV prevention, human rights and economic justice can only succeed together.
- Ken Mwehonge, advocacy program officer at HEPS-Uganda, confronts the question of paying for PrEP in his blog post, PrEP Won’t Protect if it’s Price Out of Reach.
- Back in September, our Self-Testing is on the Map blog highlighted recent studies that brought insight into how HIV self-testing could work. In December, WHO issued new guidelines on HIV self-testing and partner negotiation. The updated publication has new recommendations, additional guidance on scaling up self-testing and the complete guidelines. And just last week, IAPAC launched Recommendations for the Rapid Expansion of HIV Self-Testing in Fast-Track Cities. Stay tuned for more updates about where and how self-testing might fit into programs.