On July 17th, the World Health Organization Released new consolidated guidelines on HIV testing services that bring together new and existing recommendations on the intervention that WHO calls “the gateway to prevention services and life-saving treatment and care.” HIV testing is also the first “90” in the UNAIDS Fast Track targets that seek to have 90 percent of people living with HIV tested, 90 percent of those individuals tested on ART, and 90 percent of those on ART virologically suppressed by 2020. Given that WHO estimates just 51 percent of people living with HIV know their status, there’s much work to be done on the testing front. The new consolidated guidance provides recommendations for lay provider testing (e.g., not by a medical professional) and advises countries on how best to target.
AVAC will be delving into various aspects of the advocacy, policy and implementation landscape around testing in P-Values posts in the coming months. In this blog, by veteran HIV journalist Mark Mascolini, we take a look at self-testing—an intervention that doesn’t yet have full WHO guidance, but is on the horizon.
How would you rate a personal diagnostic system that’s accurate, easy-to-use, private, and completely confidential? Five stars, perhaps, until you learn that it costs more than many who need it most say they can pay, misses all diagnoses in a key disease period, and may inspire false—and risky—confidence. That quick take on the pros and cons of HIV self-testing distills a slowly swelling data cache, a World Health Organization (WHO) Technical Update, and two well-reasoned analyses of new technologies that could change the way many high-risk people learn they carry HIV and may even limit HIV transmissions. But research has yet to nail down whether the clear benefits of self-testing outweigh potential drawbacks. In its new guidelines on HIV testing services WHO says that there “promising evidence” for the acceptability of self-testing and recommends implementation through country demonstration projects and pilot programmes, but stops short of a general recommendation. For this, WHO says it will wait for data from several trials whose results are expected in 2015/2016.
In the meantime, though, there’s a wealth of information for advocates and activists to consider.
Possible pluses and minuses of HIV self-testing
|
Pluses |
Minuses |
|
Privacy |
Cannot detect early infection |
|
Anonymity |
Requires self-motivation for follow-up |
|
Ease of use |
Misunderstanding of procedure, interpretation |
|
Accuracy |
Mental distress over positive result |
|
Testing option for high-risk people |
Cost impact on access |
|
Mutual testing of sex partners |
Partner coercion |
|
Easier repeat testing, for example, for PrEP |
Condom-free sex after negative result |
|
Wider HIV testing lowers late-diagnosis rate |
Missed opportunity for STI screening |
Where does testing fit in to “ending AIDS??
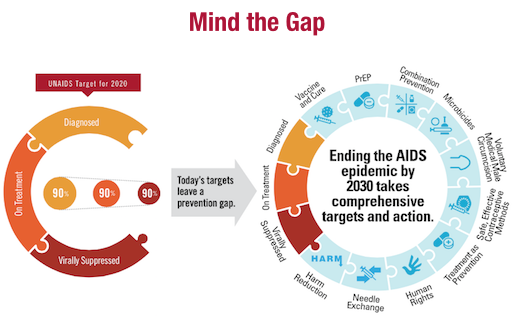
Testing is the cornerstone of the UNAIDS launched the 90-90-90 initiative, which aims to ensure that 90 percent of everyone living with HIV know their HIV status by 2020, and that 90 percent of those individuals are on ART and 90 percent of individuals on ART are virologically suppressed.
Just achieving the first 90—the testing goal—is a major undertaking. UNAIDS estimates that that 54 percent of people living with HIV across the globe don’t know they’re infected, To reach that goal, many countries are launching plans to massively expand HIV testing—and the draft versions of PEPFAR country operation plans that circulated earlier in 2015 bore this out with funding and detailed national planning. Much of this expansion is focused on linking people who test positive to ART; there is far less discussion of how testing could be used as an entry point for additional prevention services, including PrEP, for people who are HIV negative. But for PrEP-watchers, this is a key concern. Leveraging testing expansion as an entry point for effective prevention could revolutionize HIV prevention; in addition, safe and effective PrEP use requires HIV testing on a regular basis to ensure that the mono- or dual-therapy is not being used by someone who has acquired HIV.
Is self-testing a partial solution?
With all of this context, the question remains: How can public health authorities expand HIV testing when many high-risk people avoid it because they fear stigma and discrimination—especially if they test positive? HIV self-testing—usually done at home—could be a big part of the answer because it’s completely private. All HIV self-tests are easy to use, though users must be able to read and understand instructions. Studies of the oral HIV self-test found that more than 80 percent of users understood how to use the kit and interpret the results. Research involving untrained self-testers found low operator error rates ranging from 0.37 to 5.4 percent.
No one doubts the demand for confidential self-testing systems. Two recent systematic reviews of self-test studies in the US, Europe, Asia, and Africa figured that 70 percent of potential users in one analysis and up to 84 percent in another found current HIV self-test kits acceptable, and high proportions thought them easy to use. And it seems clear that home-use kits can reach high-risk people. An FDA modeling study of an oral fluid diagnostic test predicted that 2.8 million people would use the test in 1 year and that it would prevent 4,000 new HIV transmissions. Half of the participants in another analysis said the self-test was their first HIV test. In countries that license HIV self-tests, kits can be bought off the shelves of many pharmacies or purchased online. Vending machines may one day dispense HIV self-tests.
Ready access to these tests, and their confidentiality, could encourage repeat use by high-risk people and facilitate the regular HIV testing necessary for effective PrEP. (UNITAID issued a call for proposals on PrEP that could include an HIV self-test.) A trusted self-test could promote mutual testing by sex partners. One systematic review determined that 80 to 97 percent of test users reported partner testing. Some research suggests rapid self-test kits will enable joint testing by new partners and could alter subsequent sexual behavior. Research confirms the intuitive assumption that wider HIV testing cuts the late-diagnosis rate and thus improves individual HIV care.
Current self-test devices use either a spot of blood from a finger pin-prick or oral fluid swabbed from the mouth. A systematic review found that potential users consistently preferred the oral test over the finger-prick. The oral test may yield an incorrect result a bit more often than the blood tests (see table below), but all tests licensed by regulatory agencies are highly reliable. WHO cautions though, that user errors and local HIV prevalence can affect self-test accuracy. People who want to buy an HIV test online should make sure regulators have licensed the test they seek because unlicensed tests may be less accurate.
Cost and inability to detect HIV in the early months of infection are two prime drawbacks of current HIV self-tests. For example, two licensed tests in the United States cost about US$40 per kit, while a test licensed in the United Kingdom in 2015 costs £30 (USD$46) Most survey respondents in self-test studies said they would not pay more than US$20 for such a test. In many regions, the poorest people are those with the highest HIV burden, so high cost could undercut the HIV-preventing potential of self-testing.
All current self-tests detect HIV antibodies, which take time to develop in a newly infected person. Almost everyone will have detectable antibodies within three months of infection, but before that someone can be HIV-positive and still test negative on an HIV self-test kit or other HIV antibody tests. Health experts fear that a negative self-test in the first weeks of HIV infection—when viral load and the potential for HIV transmission are highest—could lead some people to feel safe having sex without a condom. Because self-tests detect antibodies, they cannot be used in infants, who carry maternal HIV antibodies even if they are HIV-negative themselves.
The newest HIV self-tests give results in 15 to 20 minutes at home. Some health authorities fear that people who test positive at home may be less likely to seek counseling (which self-test makers facilitate) and less likely to enter care than people who test positive in a center where health workers read rapid-test results and counsel people immediately. If people self-test because they fear stigma, the same fear may keep them from seeking counseling or care. People with limited phone or internet access, some worry, would have a harder time seeking counseling and starting care. And if sexually active people can test themselves for HIV at home, they may be less likely to get tested regularly for other sexually transmitted diseases.
Another conceivable drawback of self-testing is that partners will coerce their mates into testing themselves and even abuse them if they don’t or if they test positive. Data supporting or disproving these hypotheses remain limited, and WHO reports no accounts of human rights violations or violence associated with self-testing.
Comparing three representative HIV self-tests
|
|
Home Access HIV-1 Test System |
OraQuick In-Home HIV Test |
BioSure HIV Self Test |
|
Licensed |
1996 in USA |
2012 in USA |
2015 in UK |
|
Where can I get it? |
Drug stores |
||
|
How it works |
Blood sample from finger-prick sent to lab. |
Oral fluid from mouth swab put in testing device. |
Blood sample from finger-prick put in testing device. |
|
How long does it take to get results? |
Three to seven business days after you mail test sample.* |
20 to 40 minutes |
15 minutes |
|
What happens next? |
If you test positive, the lab runs a second confirming test. |
If you test positive, you must go to testing center or medical clinic for a confirming test. |
If you test positive, you must go to testing center or medical clinic for a confirming test. |
|
What else does the testing company provide? |
If you test positive on a first test and follow-up test, company provides confidential counseling and referral to an HIV provider in your area. |
If you test positive on a first test, company provides confidential counseling and referral for a confirming test. |
If you test positive, company offers online assistance to find testing center for a confirming test. |
|
How soon after HIV infection will the test show a positive result? |
Test detects HIV antibodies, not HIV itself. Antibodies take 3 to 6 months to develop after infection. |
Test detects HIV antibodies, not HIV itself. Antibodies take 3 to 6 months to develop after infection. |
Test detects HIV antibodies, not HIV itself. Antibodies take 3 to 6 months to develop after infection. |
|
How accurate is the test? |
More than 99.9% of people who are HIV positive will get a positive result. More than 99.9% of people who are negative will get a negative result. |
About 92% of people who are HIV positive will get a positive result. That means up to 1 in 12 positive people may get a negative result. Up to 99.98% of people who are negative will get a negative result. About 1 in 5000 results will be false-positive. |
99.7% of people who are HIV positive will get a positive result, while 99.9% of people who are negative will get a negative result. |
|
What HIV strains can it detect? |
HIV-1 |
HIV-1 and HIV-2 |
HIV-1 and HIV-2 |
|
How much does it cost? |
About $40 |
About $40 |
About £30 |
*Or on day sample arrives in lab with more expensive express service.
A WHO Technical Update concludes that “HIV self-testing has the potential to increase access to HIV testing including among people living with HIV without their knowledge, and those who are in need of HIV care, treatment and support.” The WHO document offers a clear summary of policy and regulatory considerations for policy makers and implementers.