Rob Newells is the newly appointed Executive Director of AIDS Project of the East Bay. He is minister and founder of the the HIV program at Imani Community Church in Oakland and has been an AVAC PxROAR member since 2012. This blog is one in a series written by community scholars who attended CROI 2016.
I have a love-hate relationship with the annual Conference on Retroviruses and Opportunistic Infections (CROI). The 12-hour days of high science can be overwhelming, and even after being deliberate about building down time into my schedule, I still crashed and burned before the end of Day 3. (It took the entire week to adjust to the time difference between East and West coasts, and after the daily 7 am Community Educator Breakfast Updates, I struggled to stay awake and alert for the morning plenary sessions.) But I survived!
There are always major headlines coming out of meetings like CROI. As a biomedical research advocate, my inner nerd gets super-excited about things like Phase 2 study results from MTN 017 (a rectal microbicide study), but at CROI I’m a community educator. I try my best to take off my research nerd hat for a few days and tune my ears to hear what members of my community will find useful right now. (I’ll have plenty of time and dozens of webinars to help me grasp all of the high-level science presented at CROI so that my inner nerd will be ready for additional updates during the International AIDS Conference in July.)
The week after returning to Oakland from Boston, I shared information with the staff working at AIDS Project of the East Bay (APEB) and with community members participating in a series of breakfast discussions coordinated through my ministry at the Imani Community Church in partnership with the East Bay HIV Faith Collaborative. This is what I told them:
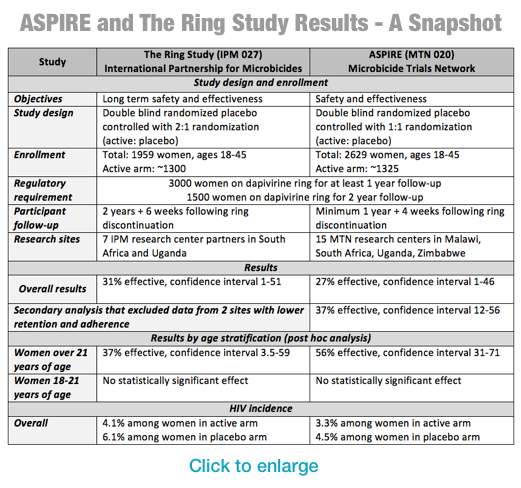
- Vaginal microbicide rings look like they’ll work. Don’t be frightened when you hear that the HIV infection rate was only reduced by about 30 percent. Remember that old 44 percent reduction in the HIV infection rate for pre-exposure prophylaxis (PrEP) when the first iPrEx study results were released just over five years ago? It gets better! With PrEP we saw that when people know the product actually works, they use it more and risk goes down. It works when you use it! Will the same thing hold true for the vaginal ring? There’s a need for open-label studies to see if women will use it more when they know it works.
- There’s reason to think injectable PrEP might work, but there are questions about how to deal with the “tail” — the period of time after injectable PrEP is terminated but there still may be low (non-protective) levels of drug in the system.
- People who use oral PrEP are generally people who are already at-risk for STIs, and they should be tested more often than every six months as is currently recommended by the CDC. (Our Medical Director at AIDS Project of the East Bay already screens PrEP clients for STIs quarterly as suggested by the research presented at CROI.)
- We talked a little about the PrEP failure case from Canada, which occurred when the PrEP user was infected with tenofovir- and emtricitibine-resistant virus. But staff and community members alike were more interested in the HPTN-073 study results showing that, with a little client-centered care coordination (C4), it’s really not so difficult to spark black men’s interest in PrEP. This was the silver lining in the cloud hovering over the community after CDC presented lifetime risk estimates indicating that half of all gay black men in the US will test positive for HIV if we don’t do something about it now. (If my community needed a wake-up call… a new reason for a sense of urgency around this HIV epidemic… a fire lit under its collective ass… This has to be it.)
Then we spent a little time talking about things I heard at CROI that probably won’t make headlines:
- Did you know that fat may stimulate HIV replication and act as a reservoir for HIV cells? How do we talk to our clients about obesity and weight loss?
- Do you really understand how much smoking while living with HIV increases risk for opportunistic infections, cardiovascular disease, lung disease and some cancers while decreasing life expectancy? What are we saying to our clients living with HIV about smoking that’s different from what we say to clients not living with HIV? (After checking in with our Medical Director, APEB will be implementing a smoking cessation program through our primary care clinic.)
- When researchers looked at people’s “Perception of Infectiousness,” the takeaway for me was that black people still don’t believe having an undetectable viral load prevents the transmission of HIV. (There are lots of conversations about medical distrust among African Americans begging to be had over and over and over again until someone figures out how to effectively address the issue.)
Another CROI is in the books (and on webcast). It will likely take months for my inner research advocacy nerd to wrap my head around all of the science, but now that my sleep pattern and weather conditions are closer to California-normal, the community educator in me is very happy.