AVAC calls for trial among women to continue with urgency and to accelerate planning for possible introduction of new option to prevent HIV
Contact
Mitchell Warren, +1 (914) 661-1536, [email protected]
Kay Marshall, +1 (347) 249-6375, [email protected]
New York City, May 18, 2020 – AVAC welcomes the news that an injectable antiretroviral for HIV pre-exposure prophylaxis (PrEP) has demonstrated initial safety and efficacy in cisgender men and transgender women who have sex with men. The US National Institute of Allergy and Infectious Diseases (NIAID), the HIV Prevention Trials Network (HPTN) and ViiV announced today that a bi-monthly injection of cabotegravir (CAB-LA) appears to be at least as effective as daily oral TDF/FTC (brand-name Truvada) at preventing HIV acquisition in HIV-uninfected cisgender men and transgender women who have sex with men. The data come from HPTN 083, one of two ongoing HIV prevention safety and efficacy trials of CAB-LA. The announcement was based on a scheduled review by an independent data and safety monitoring board (DSMB) that found that CAB-LA was providing significant protection.
“This is encouraging news for the HIV prevention field. We need additional prevention options to help people protect themselves from HIV,” said Mitchell Warren, AVAC executive director. “We now know that for men and transgender women who have sex with men, CAB-LA appears safe and effective. We look forward to the peer review publication of these data, as well as the results from the ongoing, companion trial in cisgender women, HPTN 084, in hopes that this might be a safe and effective option for all people at risk of HIV infection.”
As reported today, the DSMB recommended that all HPTN 083 trial participants be told which active drug (CAB-LA or oral TDF/FTC) they were receiving and that placebos be dropped from the study. The study will continue to completion with all participants receiving their preferred product. The DSMB also recommended that the HPTN 084 companion study continue with both active and placebo products. Both HPTN 083 and HPTN 084 are designed as double dummy, double blind studies with participants receiving both an active product and a placebo.
“Data on safety and efficacy among women, expected from HPTN 084, remain an urgent priority,” Warren added. “In many communities, women are at very high risk for HIV and have few options for HIV prevention. We cannot allow women to be left behind in the search for safe, effective and licensed HIV prevention options.”
“In addition, there is urgent work to be done to understand what HIV prevention programs and health systems need to do now in order to meet future demands of delivering a drug by injection every two months,” Warren added. “In 2018, AVAC and the Clinton Health Access Initiative (CHAI) established the Biomedical Prevention Implementation Collaborative (BioPIC) to work with a wide range of stakeholders to develop an introduction plan for long-acting injectables and other next-generation HIV prevention options. Today’s announcement makes planning all the more important if promising research results are to be translated into public health impact.”
These clinical trials are an important step in the process, but much additional work is needed. Every product has unique attributes and challenges, and there is much more to be understood about CAB-LA and the way in which it might be effectively delivered in communities and among populations where it is most needed. Understanding user preferences, health system capacity needs, the price of the product and the programs to deliver it, and the potential risk of drug resistance, amongst other issues, is necessary to move forward as quickly as possible.
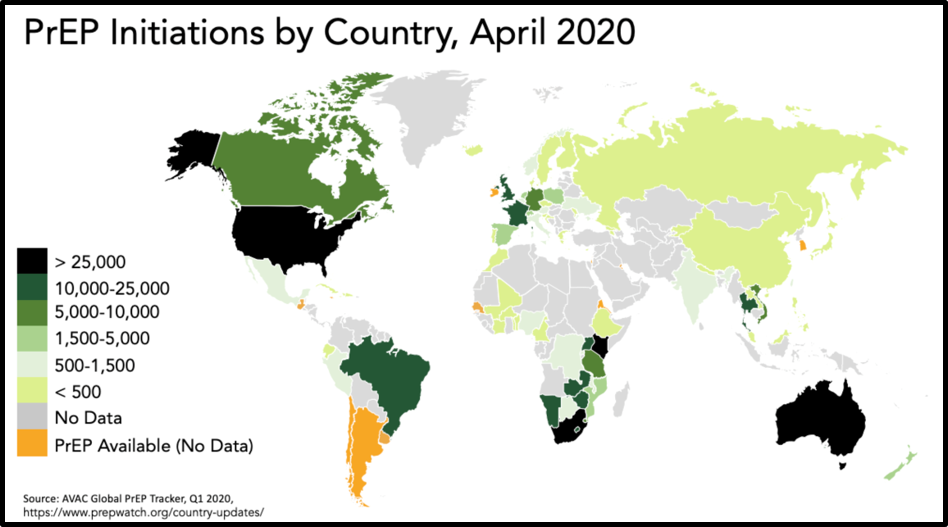
“Operational research to find out how communities and individuals can best be supported to access the drug and how health systems can be strengthened to deliver it, should it be approved for use, is a critical next step while we await complete data from all populations that would inform a regulatory submission,” said Warren. “This is essential work that can and must begin now so that we don’t repeat the same kind of delays that have slowed daily oral PrEP rollout over the past eight years.”
###
About AVAC: Founded in 1995, AVAC is a non-profit organization that uses education, policy analysis, advocacy and a network of global collaborations to accelerate the ethical development and global delivery of HIV prevention options as part of a comprehensive response to the pandemic.