Underscores need for expanded access to proven, available HIV prevention options, says AVAC
Contact
Kay Marshall, +1 (347) 249-6375, [email protected]
New York City, August 31, 2021 – Today, Johnson & Johnson and partners announced that the Imbokodo study, a large-scale HIV vaccine proof-of-concept trial also known as HVTN 705/ HPX2008, did not significantly reduce the overall risk of HIV acquisition among over 2,600 women in five sub-Saharan African countries. The Adenovirus26-based mosaic vaccine regimen was shown to be safe, but it did not meet pre-defined criteria for efficacy to warrant moving forward for longer follow-up. A companion study, the Phase III Mosaico trial, will continue.
“AVAC recognizes the enormous contribution of the 2,637 women from five countries in Southern Africa who participated in the trial, and we congratulate the trial teams at sites and across the globe for their work on a superbly run study,” said Nandisile Luthuli, AVAC’s Regional Stakeholder Engagement Manager. “We applaud Johnson & Johnson for working in collaboration with the HIV prevention community, for their leadership in HIV vaccine research and for their longstanding commitment to Good Participatory Practices (GPP) that must be continued to maintain trust in vaccines and in research.”
“We always hope that efficacy trials will show positive results that lead directly to new prevention options,” said Mitchell Warren, Executive Director of AVAC. “It is very disappointing that this particular vaccine candidate did not work in this trial, but the trial was well-conducted and got an answer quickly. HIV remains a global threat, and a safe, efficacious and accessible HIV vaccine is still needed to contribute towards curbing new infections and providing a durable end to the pandemic.”
“This is in no way the end of the search for an HIV vaccine,” added Warren. “We still hope for a positive outcome from the ongoing Mosaico and PrEPVacc studies. Yet, now more than ever, the vaccine field needs diversity and creativity — and even more collaboration — in deciding what comes next as research priorities as there are no other vaccine candidates currently on a clear track to licensure. The field must focus on new hypotheses driven by this result and the recent antibody-mediated prevention study results, both of which showed some trends towards efficacy.”
“Just as decades of HIV research paved the way for effective COVID-19 vaccines, HIV vaccine developers now need to draw on the creativity, speed, agility and decision-making of COVID-19 vaccine development in product development, trial design and regulatory pathways,” said Stacey Hannah, AVAC’s Director of Research Engagement. “AVAC calls on donors, research groups and industry to join in strategic discussions with civil society and trial communities to map out a comprehensive strategy for the future of HIV vaccine research, product development and selection, and trial designs.”
A renewed commitment to this type of engagement within the HIV vaccine field would build on lessons learned from COVID-19 vaccine development and lead to a strategy that is coordinated, appropriately resourced, includes relevant target product profiles, and commits to share data across research groups and trials.
“For the last two decades, we have seen HIV prevention trials reporting annual incidence rates of four percent or higher among women trial participants in various East and Southern African countries. Sadly, Johnson & Johnson noted a high rate of HIV infections in this trial as well. There is a moral and ethical obligation to provide women living in contexts of HIV risk with prevention options that work for them,” added Warren. “The Imbokodo study is yet another stark reminder of the need to work harder and faster to roll out effective HIV prevention options at scale to the people who need them most, and to provide appropriate support to those using prevention options, even and especially within clinical trials.”
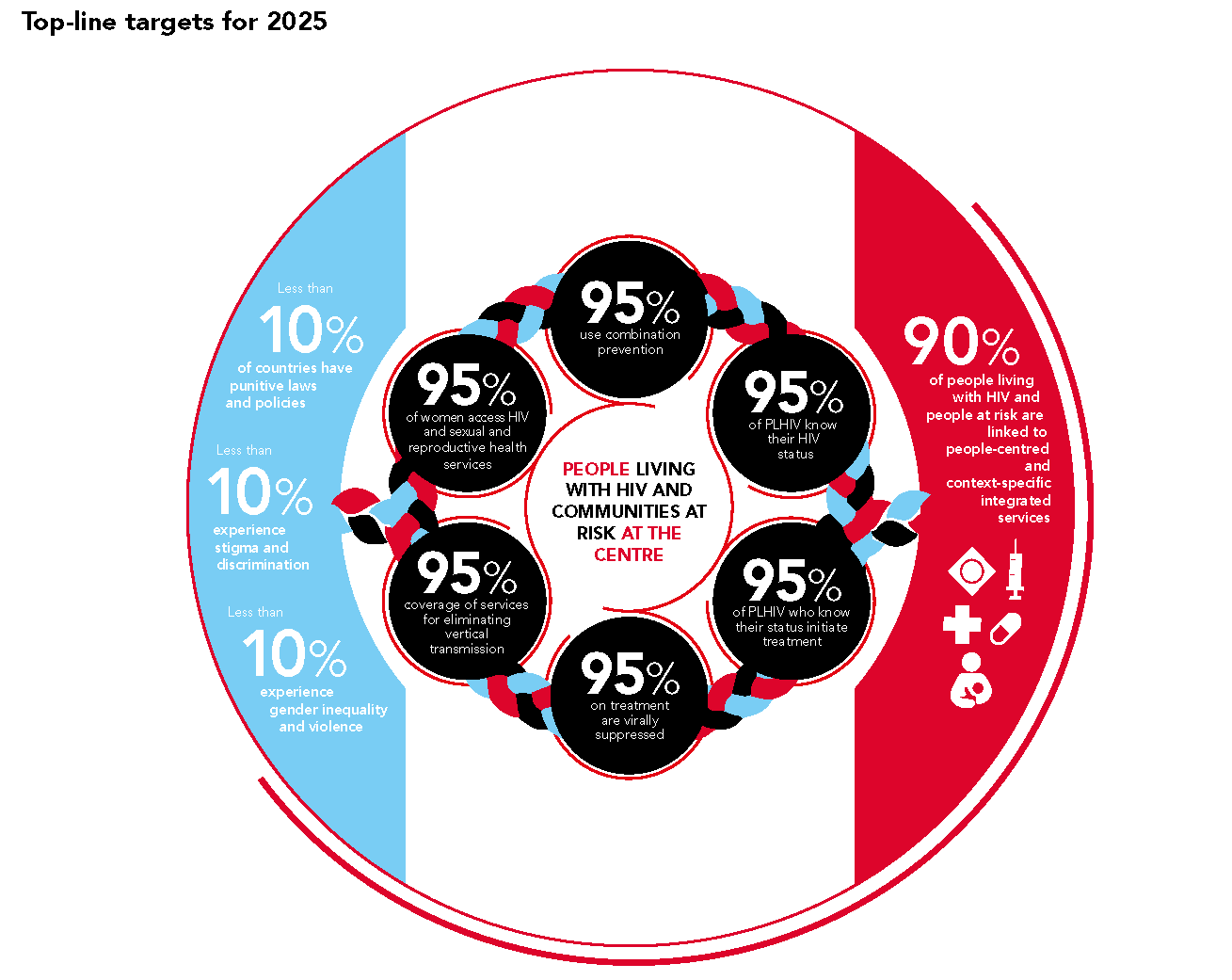
Safe and effective HIV prevention options, including male and female condoms, voluntary medical male circumcision and daily oral PrEP are all available now, but not rolled out to scale. Additional prevention options are nearing availability, including the Dapivirine Vaginal Ring and injectable cabotegravir, and several next-generation PrEP options are now entering advanced clinical trials.
“As the Imbokodo study participants return for their final visits, it is essential that they not only receive the research results, but are offered access to all available prevention options, including oral PrEP – which is available in all countries where the trial took place – and linked directly to these services,” added Luthuli. “In addition, the trial team and sponsors should explore innovative approaches to offering these trial participants the opportunity to enroll into new introduction projects offering the Dapivirine Vaginal Ring and injectable cabotegravir. The Imbokodo study team did a remarkable job of recruiting participants at high risk of HIV infection, and they now need to link the women to prevention options that work and can help them remain HIV-negative.”
The recent results of the HPTN 084 trial of injectable cabotegravir showed very low incidence rates among women in both the intervention arm and the comparative daily oral PrEP arm, making it clear that both forms of PrEP are effective prevention options. These options need to be taken to scale with urgency where they are most needed. In addition, going forward, AVAC calls for HIV prevention researchers, funders and sponsors to learn from the HPTN 084 success and better integrate these options into all future trials, even though this will require larger and more innovative trial designs.
The Imbokodo study evaluated whether an Adenovirus26-based mosaic vaccine regimen could safely and effectively reduce the rate of new HIV infections among 2,637 cisgender women in 23 sites in Malawi, Mozambique, South Africa, Zambia and Zimbabwe. Participants received a total of four doses over 12 months of either a prime-boost vaccine regimen of a mosaic viral-vectored vaccine, Adeno26.Mos4.HIV (Ad26 prime) and an aluminum phosphate-adjuvanted clade C gp140 protein (boost), or a placebo. Johnson & Johnson reported today in a press release that primary analysis of the data showed an efficacy estimate of 25.2 percent, but with a wide confidence interval that crossed zero (-10.5% to 49.3%). The press release also noted high HIV incidence rates among the women in the trial.
The Mosaico study uses a similar regimen with the same Ad26 platform for the prime vaccine, but using a different form of protein boost. The Phase III study, also known as HVTN 706/HPX3002, is currently enrolling 3,800 men and transgender people in eight countries in the Americas and Europe.
While the Imbokodo study did not provide sufficient protection to continue, there were no safety concerns with the Adenovirus26-based mosaic vaccine candidate. The Ad26 platform delivers a protein, known as an antigen, to stimulate an immune response. The platform has proven effective in other successful vaccines, including for Ebola and COVID-19. There is every reason to have confidence in the effectiveness of the Ad26-based Ebola and COVID-19 vaccines that have been important in helping to curb Ebola outbreaks and blunt the current COVID-19 pandemic. It is important to remember it is not the platform that provides protection, it is the immune reaction to the antigen within the platform. Unfortunately, HIV is a particularly challenging virus that more easily evades the immune system compared to many other viruses.
“We need an HIV vaccine to provide a durable end to the HIV pandemic, but we can’t wait for a vaccine,” added Warren. “Now is the time to go all in on providing comprehensive HIV prevention options that already exist and the programs needed to support people in using their chosen options, while also re-engaging in vaccine research. If we’ve learned one lesson from the COVID-19 response, it is that political will, sufficient funding and unprecedented cooperation in the face of a global threat is possible. HIV has been for decades — and remains — a global threat; it is past time to act boldly to confront it.”
###
About AVAC: Founded in 1995, AVAC is a non-profit organization that uses education, policy analysis, advocacy and a network of global collaborations to accelerate the ethical development and global delivery of HIV prevention options as part of a comprehensive response to the pandemic. Follow AVAC on Twitter @HIVpxresearch.