Accelerating the rollout of the full range of proven HIV prevention options depends on learning from what’s been done in the past and investing in coordination and innovation to put improved solutions in place. The Biomedical Prevention Implementation Collaborative (BioPIC) is doing just that. Over the last two years, BioPIC—a project led by AVAC with support from the Gates Foundation—has been gathering and sharing evidence on these critical lessons to ensure the next generation of HIV prevention products reaches everyone who needs and wants them with much greater speed and equity.
What We’re Learning—Highlights from 2024 Convenings
An ongoing series of think tanks, convened by BioPIC and WHO since 2021, are generating key insights for people-centered product delivery. Below, read the latest reports from these think tanks that are informing decision-making on priorities for accelerating access to PrEP. Go to the BioPIC’s page on PrEPWatch to find reports on all think tanks since 2021.
- Early Insights from EBONI and PILLAR, February 2024: Early insights from ViiV Healthcare, the manufacturer of CAB for PrEP, from two CAB for PrEP implementation studies, EBONI and PILLAR. Conducted by ViiV in the US, these are among the first studies gathering data in real-world settings. Learn more
- Taking Stock of PrEP Evidence, March 2024: An analysis of current data and priority evidence gaps. This inquiry was not focused on any one PrEP product, and its findings are informing the focus of future think tanks. Learn more
- Linking Modellers with the Latest Implementation Science Evidence, March 2024: A consideration of the latest modelling data and insights on injectable cabotegravir (CAB) for PrEP. Read about the biggest takeaways from CAB for PrEP modelling here, and learn more about the big questions that require further inquiry here
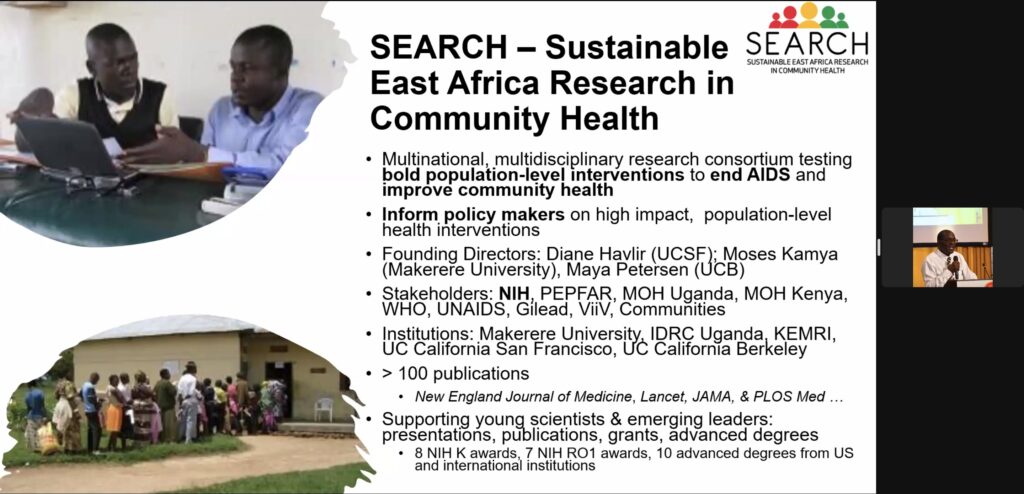
- Discussing Early Results from the SEARCH Dynamic Choice Study, April 2024: Professor Moses Kamya of Makerere University shares early insights from the SEARCH Dynamic Choice Study in Kenya and Uganda, which gave participants a choice between oral PrEP, PEP, and CAB for PrEP, and analyzes the role of choice in PrEP coverage. Watch here
- PrEP and the Role of HIV Self-Testing, May 23: Highlights from the WHO guidance on use of self-testing (HIVST) as an innovative way to increase PrEP access and coverage and further simplify PrEP delivery. Panelists also share experiences with procurement, costing, rollout and scale-up. Watch Here

As other new biomedical HIV prevention products roll out, BioPIC will continue to hold strategic convenings, identify and address evidence gaps, and work to accelerate equitable product introduction. To learn more efforts to coordinate the introduction of CAB for PrEP, check out the JIAS article Shaping and coordinating the implementation science agenda for injectable cabotegravir for PrEP: the role of the Biomedical Prevention Implementation Collaborative (BioPIC). To learn what’s needed to better coordinate rollout for not-yet-approved products in Phase III clinical trials, check out BioPIC’s Adaptable Product Introduction Framework.
We hope you will book mark these resources, and stay up to date on findings from future think tanks and webinars in 2024 on the BioPIC page of PrEPWatch.