This week brought more devastating actions from the US administration, with serious consequences for global health. From a proposed rescissions package of the current year’s funding to deep cuts in the proposed Fiscal Year 2026 budget, the end of funding to the leading NIH-funded vaccine consortia, to proposed reductions to the Global Fund match and new immigration restrictions, the threats to health, science, global partnerships, research progress, and health equity are here. Read on.
The US’ Proposed FY26 Budget and Rescissions Package Could Dismantle Decades of Progress
On Friday, the Administration released more details on the proposed Fiscal Year 2026 (FY26) US budget that was sent to Congress to inform their drafting of the final budget. As we’ve said many times over the past four months, Congress has the Constitutional power of the purse – not the President. The proposed budget slashes PEPFAR by 34% and NIH funding by 36%, for a combined total of over $5.5 billion. It further targets the Global Division of HIV and Tuberculosis (DGHT) at the US Centers for Disease Control and Prevention (CDC) by eliminating it along with other global health programming at the agency, ends funding for Gavi’s global vaccine procurement, and more.
A subsequent proposed $9.4 billion rescissions package of Fiscal Year 2025 funds that were already Congressionally appropriated but not spent was shared by the President on Tuesday. This package would eliminate over $900 million from global health programs, with OMB Director Vought refusing to rule out rescission cuts to PEPFAR. This package also seeks Congressional approval to codify, or make legal, the unlawful dismantling of USAID, which was initiated through presidential executive order and the reckless actions of DOGE. The House is expected to vote on this package soon.
IMPLICATIONS: Budgets are not just about money; they clarify priorities and policies. The proposed FY26 budget and rescissions package have far and deep implications for health, science, and research in the US and around the world. They would dismantle the architecture for global health, including health programs and research that have broad bipartisan Congressional and public support, and which support the government’s stated aim of keeping Americans and the world safer, healthier and more prosperous.
READ:
- AVAC Denounces White House Effort to Codify DOGE Cuts to Health, Research and Foreign Assistance—AVAC
- Trump Budget Request Retreats on Ending the HIV Epidemic—PrEP4All
- Trump budget request and rescission plan slashes global health funding—Devex
- Trump wants Congress to slash $9.4B in spending now, defund NPR and PBS—News From the States
- Trump Budget Eliminates Funding for Crucial Global Vaccination Programs—The New York Times
- Exclusive / GOP divide looms over scrapping Bush-era HIV program—Semafor
- Congress finally gets Trump’s request to codify DOGE cuts to NPR, PBS, foreign aid—Politico
- WH budget chief pressed on PEFPAR funds, says Africa ‘needs to absorb more of the burden’—The Hill
NIAID’s Consortia for HIV/AIDS Vaccine Development (CHAVD) Will Not Be Renewed
On Friday, news came that the National Institute of Allergy and Infectious Diseases (NIAID) will not renew funding for the Consortia for HIV/AIDS Vaccine Development (CHAVD) when they expire next June. Founded in 2005, the CHAVD programs – based at Duke University and Scripps Research Institute – have been instrumental to advancing HIV vaccine research and development, contributing to progress toward an HIV vaccine and other scientific innovations.
IMPLICATIONS: The shutdown of CHAVD and broader NIH pullback from vaccine research, along with the constrains on funding for the Advancing Clinical Therapeutics Globally for HIV/AIDS and Other Infections (ACTG), the HIV Prevention Trials Network, the HIV Vaccine Trials Network and the Adolescent Medicine Trials Network for HIV/AIDS Intervention, represent a massive – and destructive – shift in research funding. These actions squander a decades-long investment in the search for a preventive HIV vaccine, just as these efforts are gaining momentum.
READ:
- ‘Devastating’: NIH cancels future funding plans for HIV vaccine consortia—Science
- Trump Administration Ends Program Critical to Search for an HIV Vaccine—The New York Times
Global Fund Match Requirement
In the US State Department’s justification of the President’s proposed FY26 budget, Secretary of State Marco Rubio notes that “should the Administration decide to provide contributions to the Global Fund in FY26, it would ensure the United States is only contributing its fair share by leveraging $1 from the United States for every $4 from other donors, instead of the current $1:$2 matching pledge.”
Under the Global Fund match requirement, the US contribution can only be unlocked after other donors deliver on the pledges they have made. This requirement leverages American generosity to get other donors to step up.
IMPLICATIONS: If the US Government changes the Global Fund match requirement from 1:2 to 1:4, according to Friends of the Global Fight, this would reduce the leverage power of the US contribution to the Global Fund, lower overall funding to fight AIDS, TB and malaria, slow down progress on transition to country self-reliance and limit the influence of the US in Global Fund decision-making.
READ:
- The enduring impact of the 1:2 match requirement—Friends of the Global Fight
- Congressional Budget Justification, Department of State, Foreign Operations, and Related Programs—US Department of State
President Announces Restrictions and Suspensions of Foreign Nationals from 19 Countries
The President issued a new immigration proclamation restricting or fully suspending entry into the United States for foreign nationals from 19 countries, including Afghanistan, Burma, Chad, Republic of the Congo, Equatorial Guinea, Eritrea, Haiti, Iran, Libya, Somalia, Sudan, and Yemen, while partial restrictions apply to Burundi, Cuba, Laos, Sierra Leone, Togo, Turkmenistan, and Venezuela.
IMPLICATIONS: In conjunction with the cancellation of US funding for research and partnerships with foreign partners, and US withdrawal from multilateral institutions, these new restrictions, which are framed under national security, will have significant implications for global health partnerships, research collaborations, and the ability of researchers, policymakers, clinicians, advocates and others to participate in collaborative work. They also signal an era of isolation, where partnerships, diplomacy, trust-building and global health take a backseat to grandstanding, isolationist politics.
READ:
Gavi Board Appointment Raises Questions
The Gavi Board of Directors appointed Mark Kevin Lloyd, who was nominated by the new US Administration as its newest member. Lloyd is assistant to the administrator for global health at the US Agency for International Development (USAID), overseeing global health and conflict prevention. He takes Atul Gawande’s seat, which is typically held for a US government representative. Historically, five seats on the Gavi board have been held by representatives from donor countries.
Gavi is in its replenishment cycle and will hold a pledging summit later this month. In 2023, the Biden administration committed at least $1.58 billion toward the new cycle. Annual congressional appropriations are required to fulfill the pledge.
IMPLICATIONS: With Gavi’s funding zeroed out in the Administration’s FY26 budget request, it’s uncertain what this new appointment signals for US engagement with Gavi going forward.
READ:
What We’re Reading
- The Gutting of America’s Medical Research: Here Is Every Canceled or Delayed NIH Grant—The New York Times
- Ending US-global health research partnerships will cost America—STAT
- Cuts to US Aid Imperil the World’s Largest HIV Treatment Program—Bloomberg
- HIV’s Most Promising Breakthrough Has Taken a Hit—The Atlantic
- The Lavender Purge—JIAS Viewpoint
- Gilead Commits to HIV Prevention Rollout for Low-income Countries Despite Funding Uncertainty—Reuters
- Uncertain Road Ahead for Lenacapavir, a New ‘breakthrough’ HIV Prevention Drug—Positively Aware
- The US Slashed HIV/AIDS Funding. Here is How Countries that Relied on it Might Adapt—STAT
- Really, Secretary Rubio? I’m Lying About the Kids Dying Under Trump?—The New York Times (opinion)
- NIH Funding Policy Deals New Blow to HIV-related Trial Networks—Science
- The US Bought $12 Million in Aid for Poor Nations. Under Trump, it May be Destroyed—Washington Post
- US May Strip Harvey Milk’s Name From Navy Vessel—The New York Times
Resources
- The Disappearing Funds for Vaccine Research, The New York Times
- US Global Health Country-Level Funding Tracker, KFF
- An Update on PEPFAR Reauthorization, KFF
- Impact Metrics Dashboard
- Advocates’ Guide: Understanding the President’s Proposed Fiscal Year 2026 (FY26) Budget and Its Implications for Science, Research and Global Health, AVAC
- Preparing for a Supreme Court Decision That Could Change Health Care Coverage for Millions of Americans, Equality Federation and CHLP (2025), CHLP
- Research Matters, AVAC, HIVMA, TAG
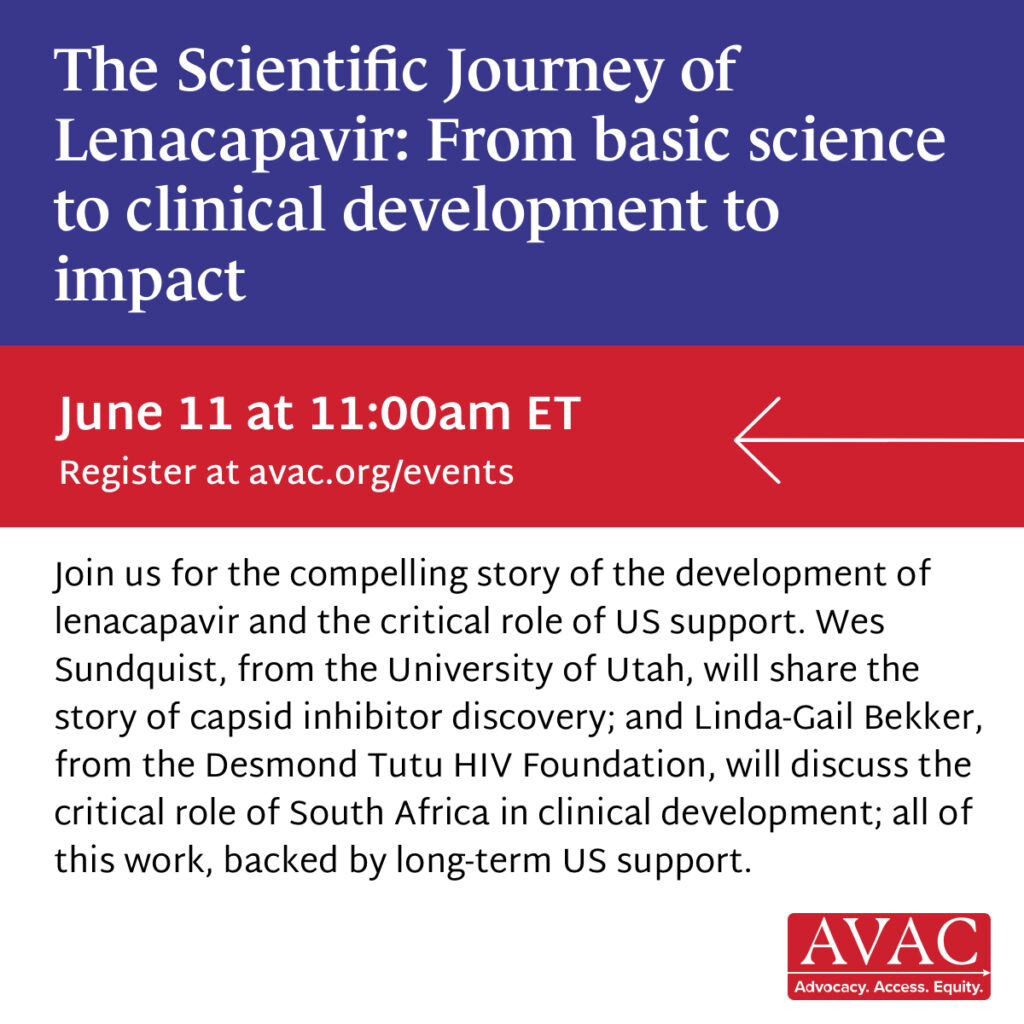
Webinar: The Scientific Journey of Lenacapavir: From basic science to clinical development to impact
Join us on Wednesday, June 11 at 11am ET
Learn how sustained US support from NIH discovery science to South Africa’s clinical research infrastructure made the development of LEN for PrEP possible.
Speakers include:
- Wes Sundquist (University of Utah), on the early-stage science behind capsid inhibitors.
- Linda-Gail Bekker (Desmond Tutu HIV Foundation), on the PURPOSE 1 trial in South Africa, where not a single HIV infection occurred.