New York, NY, October 2, 2024 — AVAC welcomes Gilead Sciences’ announcement in granting multiple, non-exclusive licenses to generic manufacturers to produce lenacapavir, their investigational twice-a-year injectable for PrEP, while it is still in clinical trials. This reflects longstanding community advocates’ calls to speed up access to PrEP options immediately following regulatory approval.
On October 2, Gilead Sciences announced their plan to work with six generic medicines manufacturers to produce and market injectable lenacapavir for PrEP in 120 countries. This process of granting licensing agreements with generic manufacturers prior to regulatory submissions could reduce the time to market for generic products by up to three years.
“Today’s announcement from Gilead is positive momentum in moving forward with injectable lenacapavir for PrEP. But while voluntary licenses are essential, they are not sufficient on their own to translate exciting science into public health impact,” said Mitchell Warren, AVAC’s executive director. “The six licenses announced today demonstrate that the field is learning what needs to go faster, and pharmaceutical companies are listening and acting.”
“This is notable improvement both in timelines for licensing and in geographic coverage, with LEN licenses being granted before regulatory approval, compared to the two-year gap after approval for injectable cabotegravir. Additionally, the six generics for LEN come from three different countries, whereas the three cabotegravir licenses were concentrated in one country. Expanding manufacturing across multiple regions can hopefully further enhance efforts to accelerate global access,” Warren added.
However, key countries with significant HIV incidence, including several of those hosting the PURPOSE 2 trials of lenacapavir, are left out of the license geographies. This challenges the field’s ability to use this new option at the scale needed to drive down HIV incidence as quickly as possible to meet global targets. In addition, the price of lenacapavir for prevention – for both the originator product and the future generics – is still unknown, another critical piece of information in building a sustainable, impactful market.
Various cost-effectiveness analyses have shown that injectable PrEP must be priced in the range of generic daily oral TDF/FTC to be considered cost-effective. Modeling studies suggest that the generic price of LEN for PrEP could be as low as $100 per person year of protection, but only when the number of vials produced is equivalent to those needed for one million LEN users.
This represents a significant increase in the current PrEP market and would require scaling up additional investment in product procurement and programming by donors and governments. While this may not be possible at product launch, the field needs to collaborate to reach this price point as quickly as possible and then move to the price of daily oral PrEP, as the number of LEN for PrEP users rises to over ten million people per year.
To reach these price points, it is essential to build volume in the global market with supplies from Gilead at close to $100 per person per year of protection beginning next year. Simultaneously, donors must procure and program large quantities and support generic manufacturers to prepare for production at scale, with market entry by 2027 to catalyze even lower prices.
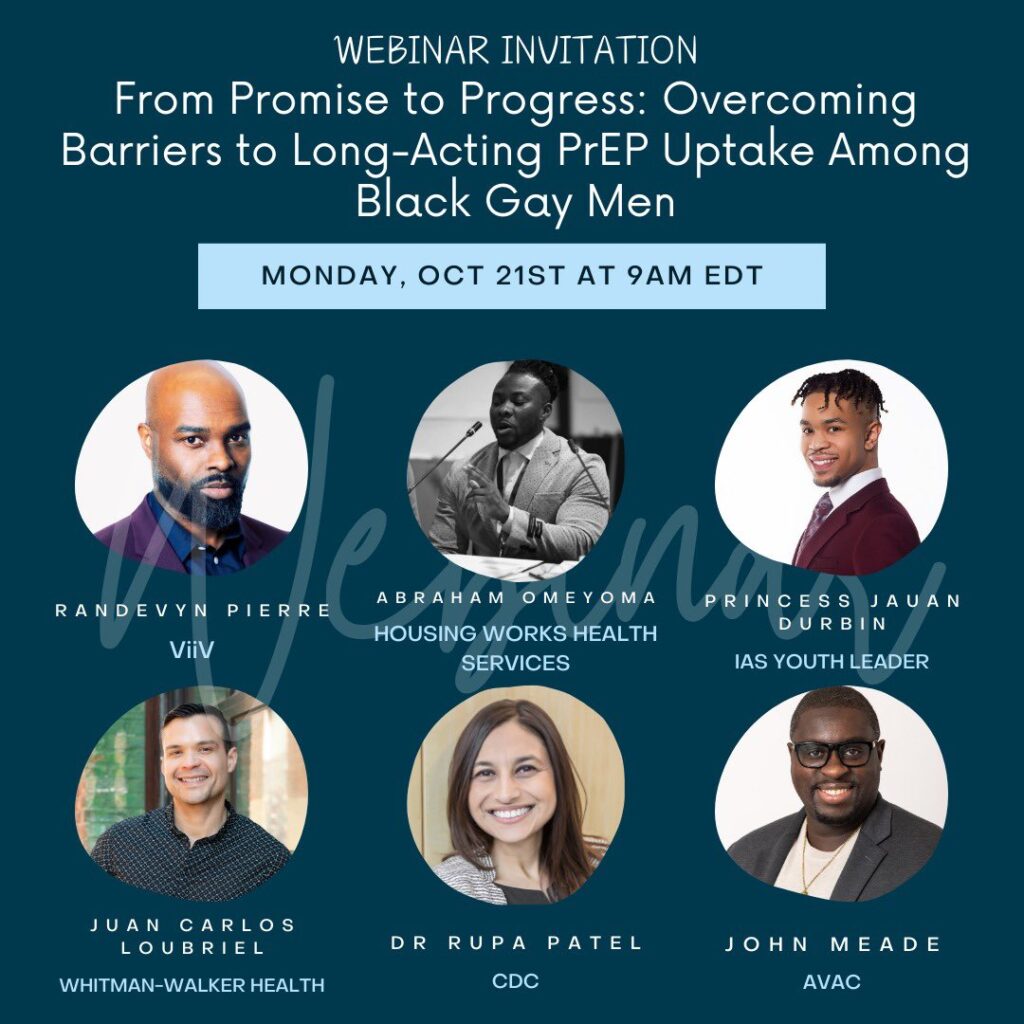
“Advocates must push for equitable and speedy PrEP access, including pricing transparency from Gilead and generics, accelerated investments by donors to design and implement integrated programs that offer LEN as part of choice of product and service delivery models, for everyone, everywhere, based on public health imperatives, and not on World Bank country classifications or geographical location,” said Wawira Nyagah, AVAC’s director of product introduction and access.
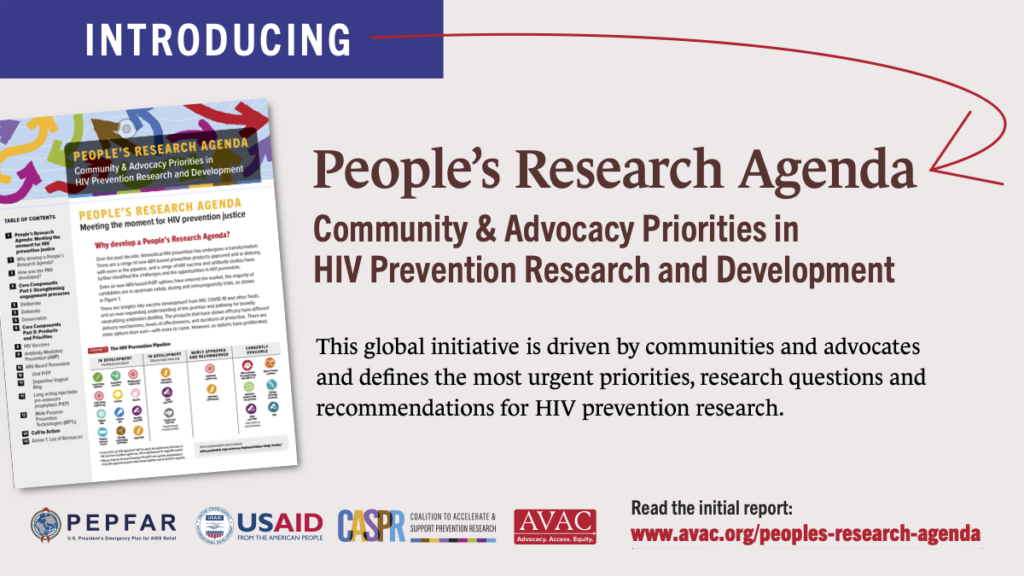
AVAC will continue to monitor the research, approval processes and product implementation of lenacapavir as part of its quarterly Long-Acting PrEP Status Updates. Please read our Lens On LEN Advocates’ Guide, which will be updated as the process toward lenacapavir access moves forward and stay tuned for our forthcoming comprehensive plan to accelerate introduction and access.
About AVAC
AVAC is an international non-profit organization that provides an independent voice and leverages global partnerships to accelerate ethical development and equitable delivery of effective HIV prevention options, as part of a comprehensive and integrated pathway to global health equity. Follow AVAC on Twitter @HIVpxresearch; find more at www.avac.org and www.prepwatch.org.