Building on priorities from the 2024 People’s Research Agenda for ARV-based prevention, this 2025 update captures how the field has evolved in the past year.
State of the Field: PRA 2025 Update
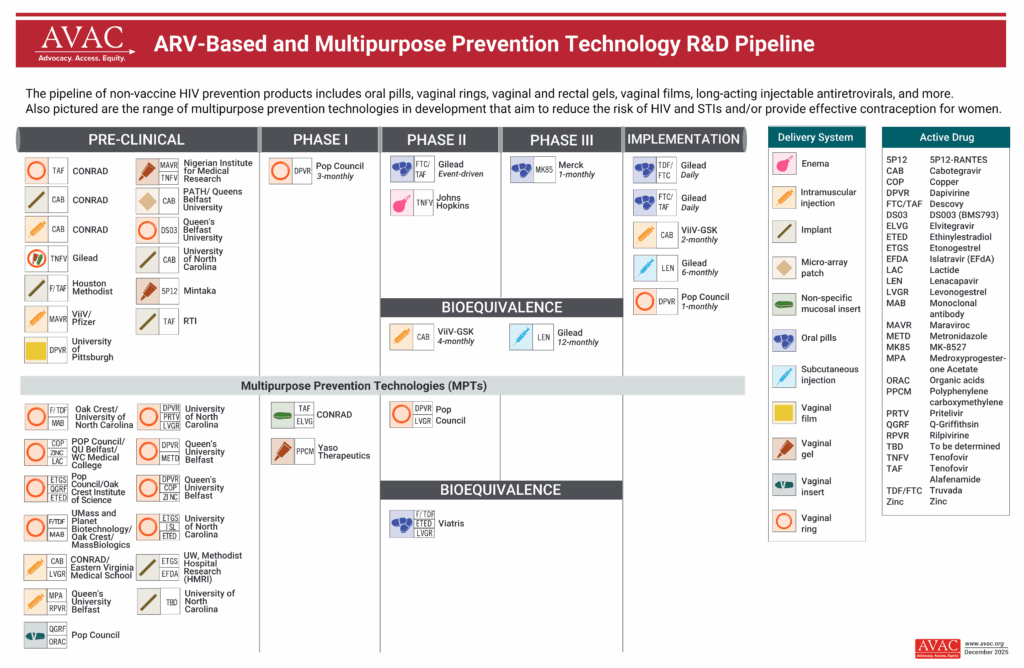
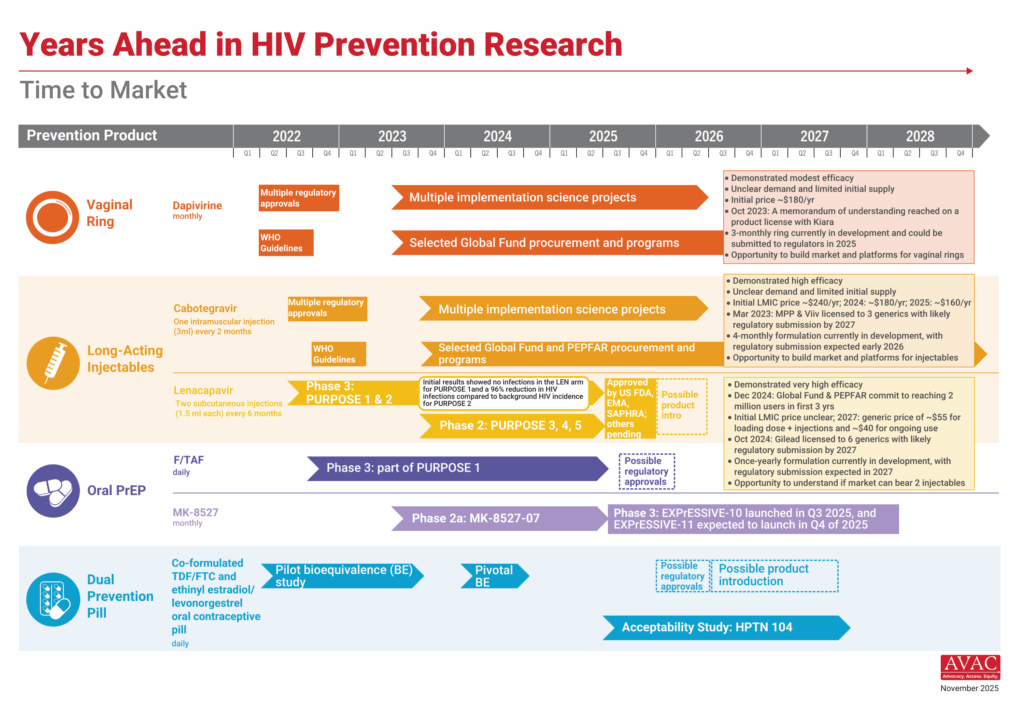
The 2025 landscape for ARV-based prevention has seen significant momentum in long-acting innovations, with scientific advances across both injectable and oral delivery platforms. Key milestones include:
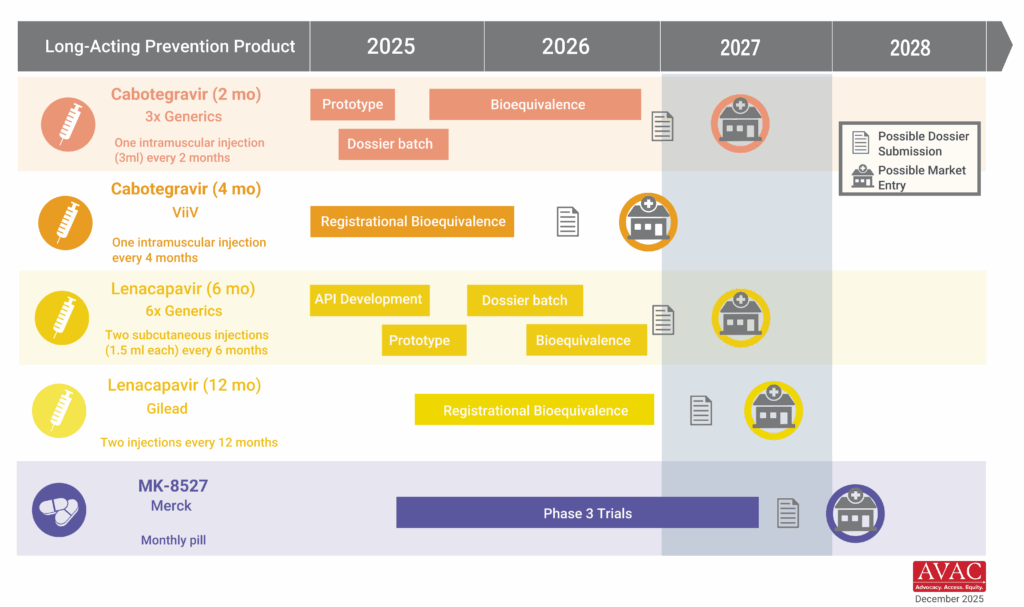
- The rapid regulatory approvals, WHO guidelines, early global procurement, and accelerated, market-shaping investments in generic manufacturing to prepare for initial introduction of lenacapavir (LEN) as the first twice-yearly PrEP option.
- Full enrollment in the PURPOSE 4 Lenacapavir study in the United States examining pharmacokinetics and open-label use among people who use drugs.
- The launch of the PURPOSE 365 Phase 3 study exploring the feasibility of once-yearly dosing for LEN.
- Further cabotegravir (CAB) studies, exploring extending protection from two to four months through bioavailability studies, signaling a broader shift toward even longer-acting products that could dramatically reduce dosing frequency and transform prevention delivery systems.
- Initiation of the EXPrESSIVE program, comprised of two Phase 3 trials across 17 countries, testing a once-monthly pill that could offer a low-burden oral alternative for individuals who prefer pills but not daily use.
- Evolution in R&D for a vaginal ring, with a 90-day dapivirine ring demonstrating superior drug release compared to the one-month version, a critical step toward extended duration.
The emergence of multiple ARV-based options presents both opportunities and critical policy and programmatic questions about how governments will prioritize and allocate resources while safeguarding user preferences and choice.
The year has also revealed serious vulnerabilities. Early-stage studies of products using innovative delivery mechanisms and shorter, user-controlled, and/or on-demand regimens are stalling due to funding cuts, threatening the future diversity of the HIV prevention pipeline. The PRA underscores that sustained investment, strategic prioritization, and early access planning are essential to ensure that this new wave of R&D innovation ultimately expands, not narrows, real prevention choice for women, adolescent girls, and all people affected by HIV.
2025 Gaps and Priorities
GAP 1: Limited implementation, scale-up, and optimization of existing PrEP options
Priority Actions
- Strengthen implementation and scale up of currently available PrEP options (oral PrEP, injectable CAB, and the dapivirine ring) to ensure choice, access and uptake across diverse populations.
- Balance investments across the full R&D continuum—from developing next-generation products, to implementation science for newly proven options, to the effective delivery of available products. Community-led models for differentiated service delivery must be sustained and strengthened.
- Leverage data from ongoing demonstration & implementation projects and PrEP programs to inform delivery models, refine ambitious targeting and address barriers that affect up-take, scale-up and optimization of existing prevention options.
- Develop clear messaging and communication at country levels on available long-acting injectable PrEP products (LEN & CAB) to avoid misinformation and ensure effective roll-out of each option as needed, thereby promoting informed choice.
- Rapidly address research gaps for the implementation of LEN highlighted in the WHO LEN Guidelines.
GAP 2: Diminished pipeline of next-generation PrEP products that meet short-acting, user-controlled, on-demand requirements
Priority Actions
- Better define the opportunities, needs, and demand for short-acting and on-demand products.
- Highlight the potential gaps that will remain in the global HIV response without a diverse range of options that will meet user preferences, especially of most vulnerable populations, and the related disadvantages and threats of relying too heavily on long-acting, systemic products.
- Ensure researchers receive support for preclinical and early phase programs that are focused on products filling precise unmet needs.
GAP 3: Pile-up of long-acting injectable PrEP products
Priority Actions
- Assess the market potential and end-user segmentation for multiple options of long-acting injectable PrEP to better articulate the need for various regimens, e.g., 2-month vs. 4-month vs. 6-month vs. annual.
- Minimize investment in duplicative development/licensure programs.
- Highlight priorities of key stakeholders, especially global funders, normative agencies, country-level policy makers, ministries of health, and healthcare providers in the scenario of multiple long-acting injectable options; and maximize investments aimed at developing and licensing prioritized products.
GAP 4: Potential loss of momentum and preparedness for rapid and equitable rollout of emerging prevention options
- Maintain robust stakeholder and community engagement, based on GPP, in the MK-8527 program, to prepare for moving from positive efficacy results to rollout.
- Align regulatory, funding, and access pathways early, ensuring that evidence generated in trials translates efficiently into equitable access once efficacy is established.
- Continue to document lessons learned from the introduction of new, innovative PrEP options, focusing currently on lenacapavir introduction, but ensuring platforms will be strengthened and sustained for future products, e.g., monthly oral pill.
Resources
- Getting Rollout Right This Time – insights and best practices for successful PrEP rollout
- Global PrEP Tracker – tracking PrEP initiations by country over time
- PrEPWatch.org – data, information, and PrEP resources
- WHO’s PrEP guidelines
- WHO LEN guidelines released in July 2025
- The Coalition to Accelerate Access to Long-Acting PrEP
Navigation
⮐ Return to the 2025 People’s Research Agenda
Previous Edition of the People’s Research Agenda