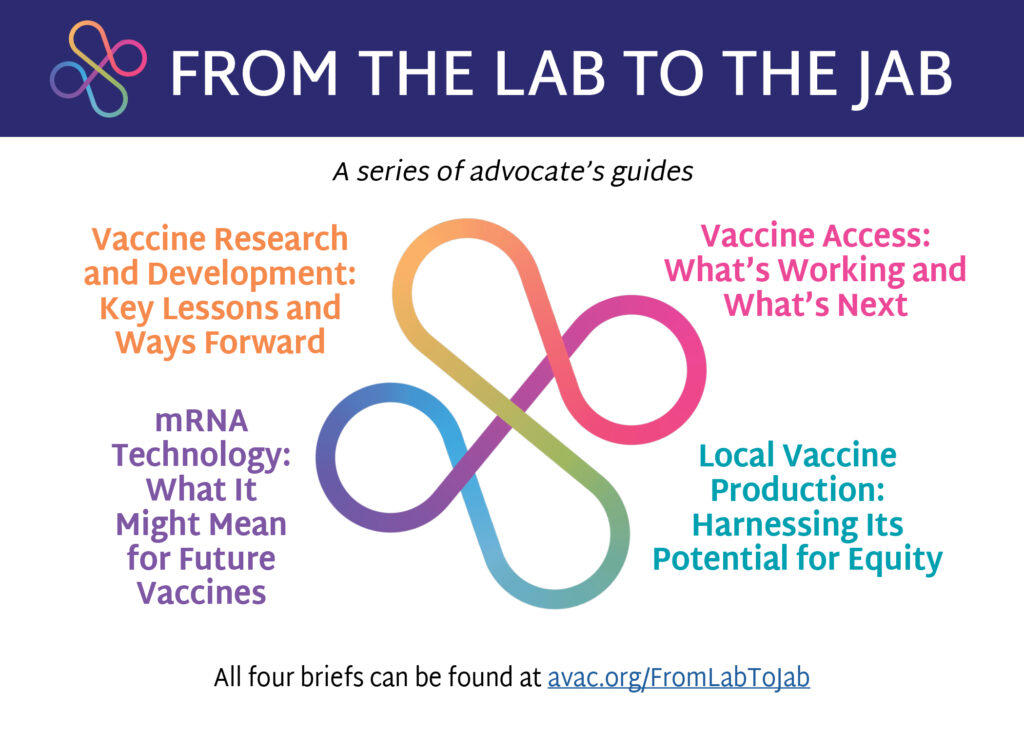
AVAC is excited to launch From the Lab to the Jab, a new series of advocates’ guides that highlight key advocacy issues to ensure equitable access to safe, effective, and affordable vaccines.
Co-created as part of our USAID-supported Coalition to Accelerate and Support Prevention Research (CASPR), with additional support from the New Venture Fund, From the Lab to the Jab issue briefs provide a roadmap for advocacy to advance the development and delivery of essential vaccines for HIV, COVID-19, tuberculosis, and other global public health threats, and approaches to ensure equitable access to these life-saving vaccines.
Go to avac.org/FromLabToJab to learn about next generation vaccine research and development; the basics of mRNA technology; initiatives that support local manufacturing; and understanding and overcoming barriers that undermine equitable access to vaccines. Each brief also highlights the advocacy needed to keep these efforts on track and in line with what communities need and want.
Stay tuned for an invitation to join the From the Lab to the Jab Webinar in January 2024, and be part of the conversation that will use these briefs to strengthen advocacy and create a roadmap to achieve key transformational priorities in global health.

