Every year, the Conference on Retroviruses and Opportunistic Infections (CROI) feels like stepping into the future of HIV science for a few intense days. The coffee is strong, the slides are packed with data, and the hallway conversations are often as important as the plenaries. This year, I left with one big question echoing in my head: How much choice is enough in HIV prevention and treatment? That question showed up everywhere — from clinical trial design discussions to the rapidly expanding pipeline of long-acting products for both prevention and treatment. Here are a few highlights from my CROI notebook.
The Era of Choice Is Here… But Are Systems Ready?
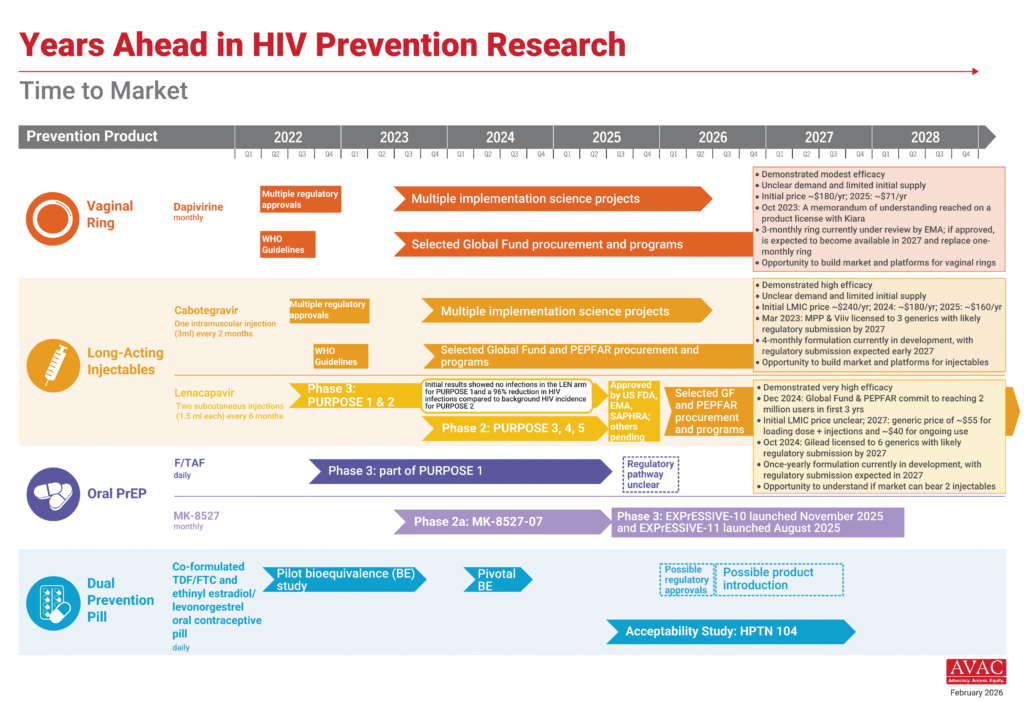
Choice continued to be a recurring theme at this year’s conference. The field and science continue to build a menu of HIV prevention options: oral pills, vaginal ring and long-acting injectables administered at varying intervals, daily, 2-monthly, 6 monthly with the potential for even longer dosing intervals in the future. But choice also raises difficult questions. At the Long-Acting/Extended Release (LA/ER) Antiretroviral Research Resource Program (LEAP) Investigator Meeting held on the sidelines of CROI 2026, Carl Dieffenbach posed a provocative one: “There will be additional prevention choices developed, but the question remains: how many choices are necessary?”
Throughout the conference, we were reminded that health systems are not always designed to handle choice or complexity. Every new product brings new requirements — supply chains, provider training, redesigned delivery models, and, importantly, funding commitments, which are increasingly limited. Still, as AVAC has highlighted in the People’s Research Agenda, the message from communities is clear: people want prevention options that fit their lives and this conversation remains relevant.
Prevention is moving toward “Ultra-Long Acting”
If you follow HIV prevention science, you’ve probably heard the term “long-acting” more times than you can count. But at CROI this year, long-acting started to feel… almost short. Researchers are now exploring so-called “ultra-long-acting” prevention. A study on cabotegravir (CAB-ULA Extended 4M) explored whether injections could move from every two months to every four months. Researchers tested a range of doses and used pharmacokinetic modelling to predict how long drug levels would remain protective. The takeaway was that a 1600 mg injection every four months could potentially maintain protective drug levels, although an initial loading dose may be needed. It remains to be seen how different injectable options with varying dosing schedules will fit into the broader prevention landscape — and whether four-months of protection is actually “ultra-long-acting” in context.
If four-months sounded impressive, another study raised the stakes. Researchers are now exploring once yearly lenacapavir for PrEP. Using data from four Phase 1 trials and thousands of drug concentration measurements, researchers modelled a regimen that could maintain protective levels of lenacapavir for 52 weeks. The proposed approach would require two oral loading doses at the start (as with the current six-monthly LEN), followed by a 3000 mg injection once per year. The upcoming PURPOSE 365 trial will test whether this annual regimen really works in people. If successful, it could reshape HIV prevention. Imagine getting your HIV prevention once a year!
Additional follow-up data from the PURPOSE 1 study on the six-monthly injectable was also shared. During extended follow-up, two infections were reported: one participant who received injections on schedule, and another who missed a dose and discontinued lenacapavir, with HIV diagnosed 16 months after the last injection. This translates to a very low HIV incidence of 0.11 per 100 person-years, reinforcing the strong protective signal seen in earlier analyses. This update also underscores an important fact: there is no perfect product.
Expanding oral PrEP options?
We heard dosing data for MK-8527, an investigational oral drug being developed by Merck as a once-monthly PrEP pill. This data wasn’t totally new as it was also presented at CROI 2025 as a poster. Researchers presented further dose-selection data supporting the EXPrESSIVE Phase 3 trials, identifying 11 mg once per month as the dose predicted to maintain protective drug levels for a full month. Phase 2 studies, combined with pharmacokinetic modelling, showed that no dose adjustments are expected for pregnant participants or adolescents weighing more than 35 kg. If Phase 3 confirms safety and effectiveness, this monthly pill could offer a compelling middle ground between daily oral PrEP and long-acting injectables, adding another important option to the growing prevention toolbox. AVAC is supporting community engagement and Good Participatory Practice implementation throughout the trials and, in partnership with local organizations and communities, created demand generation materials for the trials.
A Two-in-One Implant: Preventing HIV and Pregnancy
Another fascinating early study looked at something many advocates have long called for: multipurpose prevention technologies. Scientists are developing a long-acting implant that could deliver dolutegravir for HIV prevention and levonorgestrel for contraception. Early animal studies suggest the implant could release drugs for up to a year. It’s still early days, but the idea is powerful: one product that helps address two major health needs at once. For many women, especially in high HIV burden settings, that could be transformative.
Innovation Isn’t Just About Products — It’s About Delivery
At CROI 2026 we saw examples of innovative service delivery models that bring prevention closer to people. A randomized study among postpartum women in South Africa showed that offering dynamic choice in how PrEP is delivered improved overall PrEP use, reinforcing a simple lesson: when people can choose how to access prevention, uptake improves. In another cluster randomized trial in Kenya, researchers compared pharmacy-based PrEP delivery models with traditional clinic-based services and found that pharmacy delivery particularly when PrEP was free and supported by HIV testing services (HTS) counsellors could successfully support both initiation and continuation of PrEP. These findings echo other promising models highlighted at the conference, including pharmacy-based PrEP study in Zimbabwe, the Person-Centred Care model in Zambia, and exploration of “post-exposure prophylaxis in your pocket.” Together, they signal a growing shift in HIV prevention, moving beyond clinic walls so people can access prevention through pharmacies, communities, and other everyday points of care. How this science translate into programs will be interesting to watch.
Rethinking Clinical Trials: What If People Choose?
One of my favourite sessions explored preference in pragmatic trial designs, a fascinating approach to clinical research. Instead of forcing participants into randomization, these trials ask: What if people could choose the intervention they prefer? Pragmatic trials can measure the preference effect, do people do better when they receive what they want? It’s a simple idea with profound implications. Many questions remain, including how to address potential bias, but this is one conversation I’m eager to continue following.
A Reality Check: The Funding Cloud
Amid the scientific excitement at CROI 2026, discussions repeatedly returned to the growing uncertainty in global HIV financing. In South Africa, more than 40% of clinics reported impacts, even among those not directly funded by PEPFAR, showing how deeply interconnected HIV systems are. Speakers also warned about silent disruptions such as reduced quality of care, weakened data systems, and strained services that may not immediately show up in the numbers. As Francois Venter of Ezintsha in South Africa noted, “the science may be racing ahead, but implementation and financing must keep pace if these breakthroughs are to reach people.”
My Biggest Takeaway
CROI 2026 made one thing clear, the future of HIV prevention and treatment is expanding rapidly. We are moving toward long-acting options that will include potentially once yearly prevention, but innovation alone is not enough. The real challenge now is ensuring that these tools reach the people who need them most and that communities have the information and agency to choose what works for them. Because in the end, the future of HIV prevention will not be defined by a single breakthrough; it will be defined by choices — across many facets and by many stakeholders.